What is irritable bowel syndrome (IBS)?
Irritable bowel syndrome (IBS) is a common gastrointestinal disorder that affects the large intestine (colon). It is characterized by a group of symptoms that can include:
- Abdominal pain or discomfort
- Bloating and gas
- Constipation or diarrhea, or a combination of both
- Changes in bowel habits, such as urgency or incomplete evacuation
- Mucus in the stool
- Feeling of incomplete bowel movement
The exact cause of IBS is not known, but it is believed to be a complex interplay of factors, including abnormalities in gastrointestinal motility, intestinal inflammation, alterations in gut microbiota, food sensitivities, and stress and anxiety.
IBS is a chronic condition that can have a significant impact on a person’s quality of life, although it does not cause permanent damage to the digestive tract.
Irritable bowel syndrome (IBS): Historical perspective
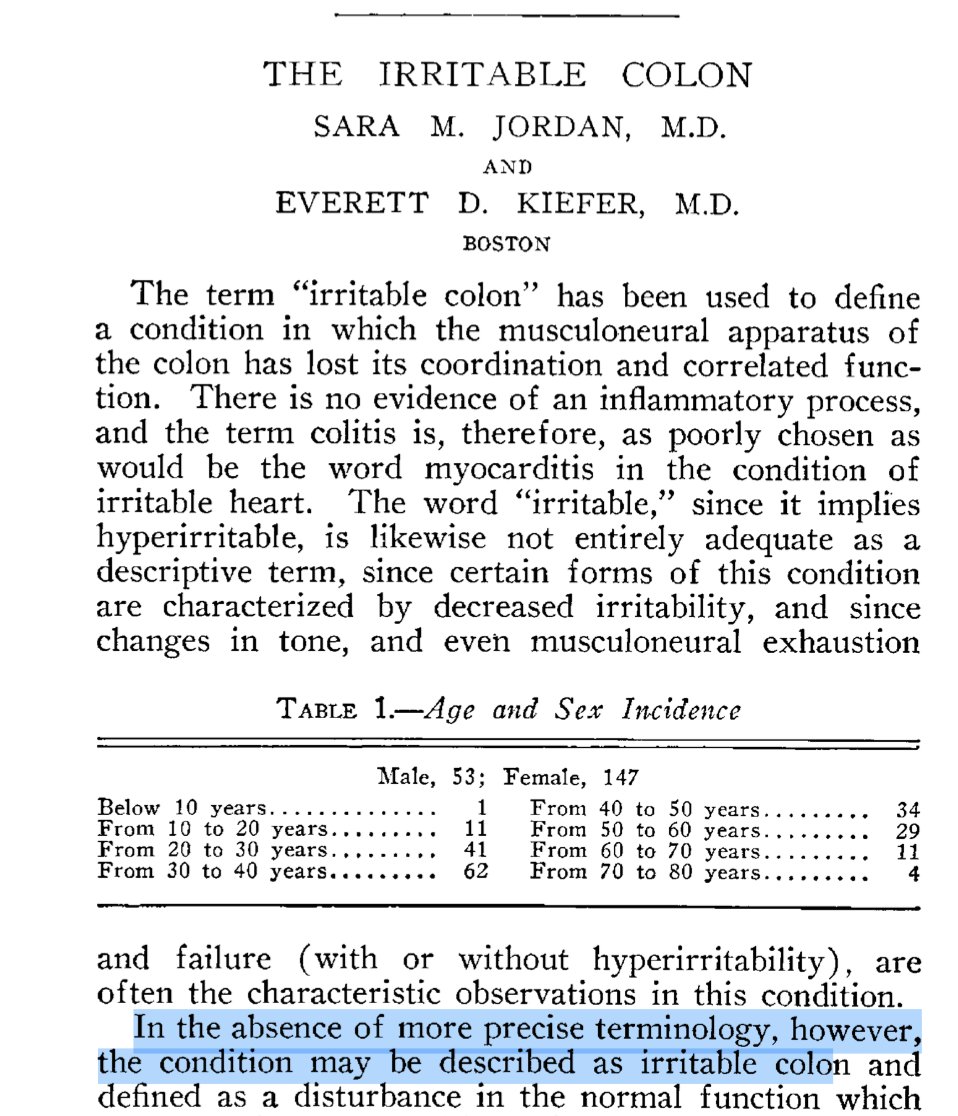
The term “irritable colon,” first described in a 1929 publication in JAMA by Sara M. Jordan and Everett D. Kiefer, marked a pivotal moment in the understanding of functional gastrointestinal disorders. Jordan and Kiefer characterized the condition as a disruption in the musculoneural coordination of the colon, leading to a loss of its rhythmic and synchronized contractions necessary for normal propulsion of contents, fluid reabsorption, and cellulose digestion. Importantly, they emphasized the absence of inflammation, distinguishing it from conditions like colitis. Despite their reservations about the adequacy of the term “irritable,” given that some cases involve decreased rather than increased irritability, the concept laid the foundation for what is now recognized as irritable bowel syndrome (IBS). Their work highlighted the complexity of the colon’s musculoneural apparatus, foreshadowing modern perspectives on IBS as a multifactorial condition involving dysregulation of intestinal motility, sensitivity, and neural function. This early understanding was instrumental in shifting the focus from purely organic pathology to a more nuanced appreciation of functional disturbances in the gastrointestinal tract.
What is the prevalence of irritable bowel syndrome (IBS)?
The prevalence of irritable bowel syndrome (IBS) varies across the world and depends on factors such as age, sex, and geographic location. According to the Rome IV criteria, which is currently used to diagnose IBS, the estimated global prevalence of IBS is approximately 11%, with a range of 9-23% depending on the population studied.
In the United States, IBS affects an estimated 10-15% of adults, with women being more commonly affected than men. In Europe, the prevalence ranges from 7-21%, with similar gender differences.
What are the Rome IV diagnostic criteria for irritable bowel syndrome (IBS)?
The Rome IV criteria are a set of guidelines used to diagnose functional gastrointestinal disorders, including irritable bowel syndrome (IBS). The Rome IV criteria for IBS diagnosis include the following:
| Criteria |
| 1. Recurrent abdominal pain or discomfort at least one day per week in the last 3 months, associated with two or more of the following: – Related to defecation – Associated with a change in the frequency of stool – Associated with a change in the form (appearance) of stool |
| 2. Symptoms started at least 6 months before diagnosis |
| 3. Symptoms are not explained by another underlying medical condition |
| 4. If alarm features are present (such as weight loss, bleeding, or fever), additional testing is needed to rule out other possible conditions |
How many subtypes of irritable bowel syndrome (IBS) are there?
According to the Rome IV diagnostic criteria, there are four subtypes of irritable bowel syndrome (IBS), based on the predominant bowel habit. These subtypes are:
- IBS with constipation (IBS-C): This subtype is characterized by a predominant symptom of constipation, with abdominal discomfort or pain, bloating, and distension.
- IBS with diarrhea (IBS-D): This subtype is characterized by a predominant symptom of diarrhea, along with abdominal discomfort or pain, urgency, and frequent bowel movements.
- Mixed IBS (IBS-M): This subtype is characterized by alternating symptoms of both constipation and diarrhea.
- Unclassified IBS (IBS-U): This subtype is diagnosed when the patient’s symptoms do not clearly fit into one of the other subtypes. Up to one-third of patients with IBS will have IBS-M or IBS-U, yet there are no licensed drugs for these subtypes.
These subtypes are not mutually exclusive, and some patients may experience symptoms of more than one subtype at different times. Additionally, some patients may experience symptoms that do not fit neatly into any of these subtypes. Gastroenterologists may use these subtypes to guide treatment decisions and to help determine which interventions may be most effective in managing a patient’s symptoms.
Is the Rome IV classification system sufficient to describe the composite nature of irritable bowel syndrome (IBS)?
Irritable bowel syndrome (IBS) is considered to be a gut-brain disorder. Patients report significantly more psychological co-morbidity than those without. Symptoms compatible with common mental disorders, such as anxiety and depression, are more common in IBS, and rates of somatoform symptom-reporting are also higher. A classification system based on bowel habit alone, as described by the Rome IV criteria, seems, therefore, insufficient to capture the complex composite nature of IBS adequately. A new classification system that also incorporates the psychological burden has recently been proposed, as shown in the Figure below.
Individuals in the clusters with the highest psychological burden, and particularly those in cluster 6 with high overall gastrointestinal symptom severity and high psychological burden, demonstrated lower educational levels, higher gastrointestinal symptom-specific anxiety, and were more likely to have consulted a gastroenterologist and used higher numbers of drugs in the previous 12 months.
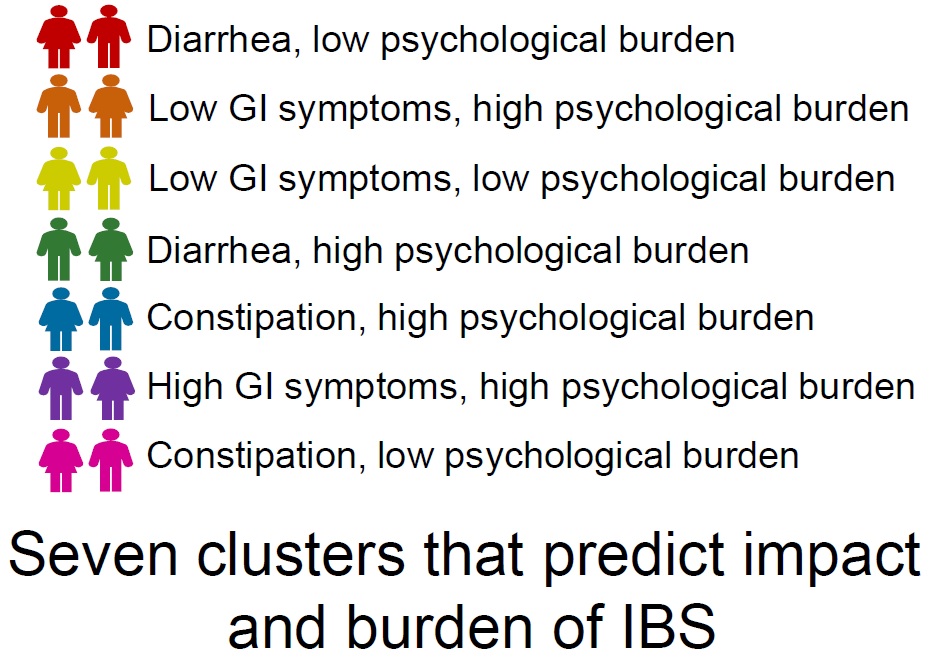
According to these clusters, there is a group of people with IBS with mild symptoms who may be best managed by reassurance, explanation of the disorder, and lifestyle and dietary advice, other groups whose symptoms are predominantly intestinal, who may be best treated with a peripherally-acting drug, a group whose symptoms predominantly extra-intestinal and psychological who may respond best to behavioral therapies, and groups with both gastrointestinal and psychological symptoms who may need combinations of peripherally- and centrally-acting drugs or peripherally-acting drugs and gut-brain behavioral therapies.
What are the alarm signs and symptoms suggesting another diagnosis is more likely than IBS?
While irritable bowel syndrome (IBS) is a common condition, it is important to be aware of potential alarm signs and symptoms that may suggest another diagnosis other than IBS. These may include:
- Rectal bleeding: This may suggest a more serious condition, such as inflammatory bowel disease or colorectal cancer.
- Weight loss: Unintentional weight loss may be a sign of a more serious underlying condition, such as cancer or malabsorption.
- Family history of gastrointestinal conditions: A family history of conditions such as inflammatory bowel disease, celiac disease, or colon cancer may increase the risk of these conditions in an individual with IBS-like symptoms.
- Age of onset: IBS typically develops in individuals under the age of 50. Onset of symptoms after age 50 may suggest a more serious underlying condition, such as colon cancer.
- Nighttime symptoms: Symptoms that wake an individual from sleep may suggest a more serious underlying condition, such as inflammatory bowel disease.
- Anemia: Low red blood cell count may suggest bleeding in the gastrointestinal tract, which may be a sign of a more serious underlying condition.
These alarm signs and symptoms do not necessarily mean that an individual has a more serious underlying condition, but rather that additional testing or evaluation may be necessary.
What causes IBS?
The exact cause of irritable bowel syndrome (IBS) is not fully understood, but it is believed to be a complex interplay of various factors, including:
- Abnormal gastrointestinal (GI) motility: IBS may be caused by changes in the normal rhythmic contractions of the GI tract, leading to either too slow or too fast movement of food and waste through the digestive system.
- Abnormalities in the gut-brain axis: The gut and the brain are connected through a complex network of nerves, and alterations in this communication may contribute to IBS symptoms.
- Intestinal inflammation: Some studies suggest that low-grade inflammation in the gut may play a role in IBS symptoms.
- Changes in gut microbiota: The gut is home to trillions of bacteria and other microorganisms, and imbalances in this microbial community may contribute to IBS symptoms.
- Food sensitivities: Certain foods and beverages, such as dairy products, wheat, and caffeine, may trigger or worsen IBS symptoms in some people.
- Stress and anxiety: Emotional stress and anxiety can affect the function of the digestive system and trigger IBS symptoms in some individuals.
IBS is a complex condition with many potential causes, and what triggers symptoms in one person may not affect another.
Are there any tests for IBS?
There are no specific tests to diagnose irritable bowel syndrome (IBS), but tests may be done to rule out other conditions that may cause similar symptoms. These tests may include:
- Blood tests: These may be done to rule out conditions such as celiac disease, inflammatory bowel disease, or thyroid disease.
- Stool tests: These may be done to rule out infections, parasites, or other conditions that may cause diarrhea or other gastrointestinal symptoms.
- Colonoscopy: This is a procedure that allows a healthcare provider to examine the inside of the colon for signs of inflammation, polyps, or other abnormalities.
- Imaging tests: These may include CT scans, MRIs, or X-rays, which may be done to rule out other conditions that may cause similar symptoms.
The diagnosis of IBS is typically made based on the presence of characteristic symptoms and the absence of any other underlying conditions. The Rome IV criteria are often used to help gastroenterologists diagnose IBS based on symptom patterns.
How can I manage my symptoms?
The management of irritable bowel syndrome (IBS) focuses on reducing symptoms and improving quality of life. Here are some tips for managing IBS symptoms:
- Dietary changes: Certain foods may trigger IBS symptoms, so it can be helpful to identify and avoid these triggers. Keeping a food diary can help identify problem foods. Some common triggers include fatty foods, dairy products, caffeine, alcohol, and artificial sweeteners. A gastroenterologists or registered dietitian can provide guidance on dietary modifications.
- Stress management: Stress and anxiety can trigger or worsen IBS symptoms. Stress management techniques, such as meditation, deep breathing, and yoga, may be helpful.
- Medications: Over-the-counter medications, such as antispasmodics and laxatives, can help relieve some IBS symptoms. Prescription medications, such as tricyclic antidepressants, can also be effective for certain types of IBS.
- Exercise: Regular physical activity can help improve digestion and reduce stress, which may help alleviate IBS symptoms.
- Probiotics: Probiotics are beneficial bacteria that can help promote a healthy gut microbiome. Some studies suggest that probiotics may help alleviate IBS symptoms, but more research is needed.
- Psychotherapy: Psychotherapy, such as cognitive behavioral therapy (CBT), can be effective in managing the stress and anxiety associated with IBS.
What medications are available to treat IBS-D?
Several medications are available to treat irritable bowel syndrome with diarrhea (IBS-D). Some examples include:
- Antidiarrheal medications: Over-the-counter antidiarrheal medications, such as loperamide (Imodium), can help reduce diarrhea and improve stool consistency.
- Rifaximin (Rifacol): Rifaximin is a prescription antibiotic that is used to treat bacterial overgrowth in the intestines. Some studies have shown that it may be effective in reducing IBS-D symptoms.
- Peppermint oil: Peppermint oil capsules may help relieve abdominal pain and discomfort associated with IBS-D. Not indicated in gastroesophageal reflux disease and in constipation.
- Butyric acid: Butyric acid is a short-chain fatty acid that plays a significant role in maintaining a healthy gut. It is produced naturally by the bacteria in our intestines during the fermentation of dietary fiber. In the context of IBS, research suggests that there may be alterations in the gut microbiota composition and metabolism, leading to reduced levels of butyric acid in the colon. This decrease in butyric acid can potentially contribute to the symptoms experienced by individuals with IBS. By increasing the levels of butyric acid in the colon, it is believed to provide various benefits like improving gut barrier function, reducing inflammation, and modulating bowel movements.
What medications are available to treat IBS-C?
Several medications are available to treat irritable bowel syndrome with constipation (IBS-C). Some examples include:
- Fiber supplements: Over-the-counter fiber supplements, such as psyllium or methylcellulose, can help soften stools and promote regular bowel movements.
- Laxatives: Laxatives, such as polyethylene glycol or lactulose, can help relieve constipation by increasing the amount of water in the colon.
- Lubiprostone: Lubiprostone is a prescription medication that works by increasing the secretion of fluid in the small intestine, which can help relieve constipation. Not available in the EU.
- Linaclotide: Linaclotide is a prescription medication that works by increasing the secretion of fluid in the colon and promoting bowel movements. Not available in the EU.
- Tegaserod: Tegaserod is a prescription medication that works by increasing the movement of stools through the colon. It was withdrawn from the market in 2007 due to concerns about cardiovascular side effects, but it was reapproved in 2019 for use in certain patients. Not available in the EU.
What medications are available to treat IBS-M?
Irritable bowel syndrome with mixed symptoms (IBS-M) can be challenging to treat because it involves both constipation and diarrhea. Although there are no licensed drugs for this subtype, some it would reasonable to recommend or test some of the following medications:
- Antidepressants: Certain antidepressants, such as tricyclic antidepressants, may be helpful in managing IBS-M symptoms. They work by altering the levels of certain chemicals in the brain and gastrointestinal tract.
- Probiotics: Probiotics are beneficial bacteria that can help promote a healthy gut microbiome. Some studies suggest that probiotics may help alleviate IBS symptoms, including IBS-M.
- Rifaximin (Rifacol): Rifaximin is a prescription antibiotic that is used to treat bacterial overgrowth in the intestines. It may be effective in reducing IBS-M symptoms.
- Peppermint oil: Peppermint oil capsules may help relieve abdominal pain and discomfort associated with IBS-M. Not indicated in gastroesophageal reflux disease and in constipation.
Are there any dietary changes I can make to alleviate my symptoms?
Yes, dietary changes can be an important part of managing IBS symptoms. Some dietary changes that may be helpful include:
- Increasing fiber intake: Soluble fiber, found in foods like oats, barley, and fruits, can help soften stools and reduce constipation. Insoluble fiber, found in foods like whole grains and vegetables, can help promote regular bowel movements.
- Avoiding trigger foods: Certain foods may trigger IBS symptoms in some people, so it can be helpful to keep a food diary to identify and avoid these trigger foods. Some common trigger foods include fatty foods, spicy foods, caffeine, alcohol, and artificial sweeteners.
- Eating smaller, more frequent meals: Eating smaller, more frequent meals throughout the day can help prevent bloating and abdominal discomfort.
- Drinking plenty of fluids: Staying hydrated can help prevent constipation and improve overall digestive function.
- Trying a low FODMAP diet: The low FODMAP diet is a specialized diet that involves avoiding certain types of carbohydrates that are poorly absorbed in the intestine. It has been shown to be effective in reducing IBS symptoms in some patients, but it should only be followed under the guidance of a healthcare provider or registered dietitian.
Not all dietary changes will be effective for all patients, and it may take some trial and error to identify what works best for each individual.
What can I do to reduce stress and anxiety, which can trigger IBS symptoms?
Stress and anxiety can be significant triggers for IBS symptoms, so managing these factors can be an important part of managing the condition. Some strategies that may be helpful in reducing stress and anxiety include:
- Mindfulness meditation: Mindfulness meditation involves paying attention to the present moment and accepting thoughts and feelings without judgment. It has been shown to be effective in reducing anxiety and stress.
- Yoga: Yoga combines physical postures with breathing exercises and meditation, and has been shown to be effective in reducing stress and anxiety.
- Cognitive-behavioral therapy (CBT): CBT is a type of therapy that focuses on changing negative thought patterns and behaviors that may contribute to stress and anxiety.
- Regular exercise: Regular exercise can help reduce stress and anxiety, as well as improve overall physical health.
- Adequate sleep: Getting enough sleep is important for reducing stress and anxiety, as well as improving overall health.
- Relaxation techniques: Techniques like deep breathing, progressive muscle relaxation, and visualization can be helpful in reducing stress and anxiety.
Not all stress reduction techniques will be effective for all patients, and it may take some trial and error to find what works best for each individual.
Can smoking affect IBS?
Yes, smoking can worsen symptoms of irritable bowel syndrome (IBS) in some individuals. Research has shown that smoking can increase the risk of developing IBS and can also exacerbate symptoms in those who already have the condition.
Smoking has been shown to have several negative effects on the digestive system, including increasing inflammation and reducing blood flow to the intestines. These effects can lead to more frequent and severe symptoms in people with IBS, such as abdominal pain, bloating, diarrhea, and constipation.
In addition, smoking can also have a negative impact on overall health, including increasing the risk of various diseases such as cancer, heart disease, and respiratory problems. Quitting smoking can be challenging, but it can have significant benefits for overall health and may also help to alleviate symptoms of IBS.
Can coffee affect IBS?
Yes, coffee can affect irritable bowel syndrome (IBS) symptoms in some individuals. Caffeine, which is present in coffee, is a stimulant that can increase the activity of the digestive system, leading to more frequent bowel movements and potentially worsening symptoms of IBS such as diarrhea, abdominal pain, and bloating.
In addition to caffeine, coffee also contains other compounds such as chlorogenic acid and N-alkanoyl-5-hydroxytryptamide, which can further stimulate the digestive system and exacerbate IBS symptoms.
However, not everyone with IBS will be affected by coffee in the same way, and some individuals may be able to tolerate moderate amounts without experiencing negative effects. Pay attention to your own body and monitor how coffee affects your symptoms. If you find that coffee worsens your IBS symptoms, you may want to consider reducing your intake or eliminating it altogether.
Can alcohol affect IBS?
Yes, alcohol can affect irritable bowel syndrome (IBS) symptoms in some individuals. Alcohol is a gastrointestinal irritant that can stimulate the digestive system and exacerbate symptoms of IBS such as abdominal pain, bloating, and diarrhea.
In addition, many types of alcoholic beverages contain high levels of fermentable carbohydrates, which can be difficult to digest and can cause bloating, gas, and other digestive symptoms in people with IBS.
Moreover, alcohol can also have a negative impact on the overall health of individuals with IBS. It can disrupt sleep patterns, dehydrate the body, and contribute to anxiety and stress, all of which can worsen IBS symptoms.
However, the effects of alcohol on IBS can vary depending on the individual and the amount and type of alcohol consumed. Some people with IBS may be able to tolerate moderate amounts of alcohol without experiencing negative effects, while others may need to avoid it altogether.
What is the role of hormones in IBS?
Hormones can play a role in the development and exacerbation of symptoms in some people with irritable bowel syndrome (IBS), particularly in women. Research has shown that changes in hormone levels can affect the gastrointestinal tract and contribute to IBS symptoms.
For example, fluctuations in estrogen levels during the menstrual cycle can affect bowel function and lead to symptoms such as abdominal pain, bloating, and diarrhea. Additionally, some women with IBS report worsening of symptoms during menopause, when estrogen levels decrease.
Hormonal birth control may also affect IBS symptoms in some women. Some studies have found that oral contraceptives may worsen IBS symptoms, while others have found that certain types of hormonal birth control, such as progestin-only pills, may be helpful in reducing symptoms.
Overall, the role of hormones in IBS is complex and not fully understood. While hormones are not a direct cause of IBS, they can contribute to symptoms in some individuals. Treatment of hormonal imbalances may be helpful in managing IBS symptoms in some cases, particularly in women with IBS.
What is the role of dysbiosis and small intestinal bacterial overgrowth (SIBO) in IBS?
Dysbiosis and small intestinal bacterial overgrowth (SIBO) are two potential contributors to the development and exacerbation of irritable bowel syndrome (IBS) symptoms.
Dysbiosis refers to an imbalance in the gut microbiome, which is the community of microorganisms that live in the digestive tract. In individuals with IBS, it is thought that dysbiosis may contribute to inflammation and alterations in gut motility, leading to symptoms such as abdominal pain, bloating, and altered bowel habits.
SIBO occurs when there is an overgrowth of bacteria in the small intestine, which can lead to symptoms such as diarrhea, bloating, and abdominal pain. Some studies have suggested that SIBO may be more common in individuals with IBS, particularly those with diarrhea-predominant symptoms.
While dysbiosis and SIBO may be contributors to IBS symptoms in some individuals, it is important to note that not all people with IBS have dysbiosis or SIBO. Additionally, treatment of these conditions is not a one-size-fits-all approach, and it is important to work closely with a healthcare provider to determine the best treatment approach for individual needs.
Treatment of dysbiosis and SIBO may involve dietary changes, probiotics, antibiotics, or other medications. The use of antibiotics in the treatment of SIBO is controversial and may not be appropriate for all individuals.
Is there a cure for IBS?
At this time, there is no known cure for irritable bowel syndrome (IBS). However, many people with IBS are able to manage their symptoms through a combination of medication, dietary changes, stress reduction, and other lifestyle modifications. The goal of treatment is to improve quality of life and reduce symptoms such as abdominal pain, bloating, and changes in bowel habits.
Can IBS lead to other health problems?
In general, IBS does not lead to other health problems or increase the risk of developing other diseases or conditions. However, people with IBS may be more likely to experience certain health problems, such as anxiety and depression, due to the impact of the condition on quality of life.
Additionally, some people with IBS may develop complications such as hemorrhoids, anal fissures, or fecal impaction due to chronic constipation. Rarely, people with IBS may experience intestinal obstruction or perforation, although these complications are very uncommon.
Will my IBS symptoms get worse over time?
In most cases, IBS symptoms do not get worse over time. However, the severity of symptoms can vary from person to person and may fluctuate over time. Some people with IBS may experience periods of remission, where their symptoms are mild or non-existent, while others may have more persistent symptoms.
Factors that can affect the severity of IBS symptoms include stress, diet, hormonal changes, and underlying medical conditions.
Can I still lead a normal life with IBS?
Yes, it is possible to lead a normal life with irritable bowel syndrome (IBS) with proper management of symptoms. While IBS can be a chronic condition that may require ongoing management, many people with IBS are able to manage their symptoms effectively through lifestyle modifications, medication, and other treatments.
Some strategies that can help people with IBS lead a normal life include:
- Understanding triggers: Identifying triggers that worsen symptoms, such as certain foods, stress, or hormonal changes, can help people with IBS avoid or manage these triggers.
- Making dietary changes: Some people with IBS may find relief from symptoms by making changes to their diet, such as avoiding certain foods or following a low FODMAP diet.
- Managing stress: Stress and anxiety can worsen IBS symptoms, so managing stress through relaxation techniques, exercise, and other strategies can be helpful.
- Taking medication: There are several medications available that can help manage IBS symptoms, including antispasmodics, laxatives, and antidepressants.
- Working with a healthcare provider: Working with a healthcare provider to develop an individualized treatment plan can be key to managing IBS symptoms and maintaining quality of life.
While IBS can be a challenging condition to manage, many people with IBS are able to lead fulfilling, productive lives with the right support and management strategies.
Are there any alternative treatments or therapies that may be helpful in managing my symptoms?
While there is limited scientific evidence to support the use of alternative therapies in managing IBS symptoms, some people find that certain alternative treatments or therapies can be helpful in reducing symptoms or improving overall well-being. It is important to talk to a healthcare provider before trying any alternative therapies to ensure they are safe and appropriate for your individual needs.
Some alternative therapies that may be helpful in managing IBS symptoms include:
- Acupuncture: Acupuncture involves the insertion of thin needles into specific points on the body to stimulate healing and reduce pain. Some studies have found that acupuncture may be helpful in reducing IBS symptoms such as abdominal pain and bloating.
- Probiotics: Probiotics are live bacteria and yeasts that can be taken as supplements or found in certain foods. Some studies have found that probiotics may be helpful in reducing IBS symptoms, particularly in those with diarrhea-predominant IBS.
- Mind-body therapies: Mind-body therapies such as hypnotherapy, cognitive behavioral therapy (CBT), and relaxation techniques may be helpful in reducing stress and anxiety, which can worsen IBS symptoms.
- Herbal remedies: Certain herbal remedies such as peppermint oil, ginger, and chamomile tea may be helpful in reducing IBS symptoms. However, it is important to talk to a healthcare provider before trying any herbal remedies, as some may interact with medications or cause side effects.
- Massage therapy: Massage therapy may be helpful in reducing stress and promoting relaxation, which can improve IBS symptoms.
Alternative therapies should not be used as a substitute for medical treatment or prescribed medication.
How can I contact gastroenterologist Dr. Zavos for an appointment?
Dr. Chris Zavos is a board-certified gastroenterologist and hepatologist, located in Thessaloniki Greece, and specifically in Kalamaria suburb, about 7 kilometres (4 miles) southeast of downtown Thessaloniki. His private office is at: Fanariou 8 street (near Aigaiou and Adrianoupoleos avenues), Kalamaria (Thessaloniki), Greece.
Thessaloniki International Airport is only 10 km away from his private office in Kalamaria and can be reached by taxi within 13 minutes from the airport.
Dr. Chris Zavos performs endoscopies at Bioclinic private hospital in downtown Thessaloniki (Mitropoleos 86 street).
You can contact Dr. Zavos at phone numbers: (+30)-6976596988 and (+30)-2311283833, or you can email him at czavos@ymail.com. Dr. Zavos responds to Greek and English languages.
References
- Kountouras J, Zavos C, et al. Efficacy of trimebutine therapy in patients with gastroesophageal reflux disease and irritable bowel syndrome. Hepatogastroenterology 2002 Jan-Feb;49(43):193-7.
- Katsinelos P, Zavos C, et al. Prevalence, bowel habit subtypes and medical care-seeking behaviour of patients with irritable bowel syndrome in Northern Greece. Eur J Gastroenterol Hepatol 2009 Feb;21(2):183-9.
- Kountouras J, Zavos C, et al. Irritable bowel syndrome associated with mitral valve prolapse and autonomic and haemostatic abnormalities in children, adolescents and adults with migraine. Acta Neurol Scand 2011 May;123(5):366-7.
- Chang L, Sultan S, et al. AGA Clinical Practice Guideline on the Pharmacological Management of Irritable Bowel Syndrome With Constipation. Gastroenterology 2022 Jul;163(1):118-36.
- Lembo A, Sultan S, et al. AGA Clinical Practice Guideline on the Pharmacological Management of Irritable Bowel Syndrome With Diarrhea. Gastroenterology 2022 Jul;163(1):137-51.
- Chan WW, Grover M. The COVID-19 pandemic and postinfection irritable bowel syndrome: What lies ahead for gastroenterologists. Clin Gastroenterol Hepatol 2022 Oct;20(10):2195-2197.
- Black CJ, Ng CE, Goodoory VC, Ford AC. Novel Symptom Subgroups in Individuals with Irritable Bowel Syndrome Predict Disease Impact and Burden. Clin Gastroenterol Hepatol 2023 Feb 27:S1542-3565(23)00158-1.
