What is constipation?
Constipation is a common digestive problem characterized by infrequent bowel movements or difficulty passing stool. It is typically defined as having fewer than three bowel movements per week, although the frequency of bowel movements can vary from person to person. In addition to infrequent bowel movements, constipation can also cause hard, dry stools that are difficult to pass, as well as abdominal pain or discomfort.
What are the causes of constipation?
There are many possible causes of constipation, including:
- Low fiber diet: Not eating enough fiber in your diet can make it difficult to pass stool.
- Dehydration: Not drinking enough water can cause the stool to become hard and difficult to pass.
- Lack of physical activity: A sedentary lifestyle can slow down the digestive system, leading to constipation.
- Medications: Certain medications such as painkillers, antidepressants, and blood pressure medications can cause constipation as a side effect.
- Medical conditions: Conditions such as irritable bowel syndrome (IBS), inflammatory bowel disease (IBD), hypothyroidism, and diabetes can all cause constipation.
- Pregnancy: Hormonal changes during pregnancy can slow down the digestive system, leading to constipation.
- Aging: As people age, the digestive system may slow down, making constipation more common.
- Ignoring the urge to have a bowel movement: Ignoring the urge to have a bowel movement can lead to constipation over time.
- Traveling or changes in routine: Changes in routine, such as traveling or changes in work schedule, can disrupt the digestive system and lead to constipation.
What types of constipation are there?
There are several different types of constipation, which can be categorized based on their causes or symptoms. Here are some of the most common types of constipation:
- Primary constipation: This is constipation that occurs without any underlying medical condition. It is often caused by lifestyle factors such as a low-fiber diet, lack of physical activity, or dehydration.
- Secondary constipation: This is constipation that is caused by an underlying medical condition, such as hypothyroidism, diabetes, or irritable bowel syndrome (IBS).
- Chronic idiopathic constipation: This is a type of constipation that lasts for several months or longer without any obvious underlying cause.
- Travel-related constipation: This is constipation that occurs as a result of changes in routine, such as traveling or changes in work schedule.
- Opioid-induced constipation: This is constipation that is caused by the use of opioid pain medications, which can slow down the digestive system.
- Slow-transit constipation: This is constipation that occurs as a result of slow movement of stool through the colon.
- Pelvic floor dysfunction constipation: This is constipation that occurs when the muscles in the pelvic floor are not functioning properly, making it difficult to pass stool.
- Functional constipation: This is a type of constipation that is not caused by any underlying medical condition, but is related to the way the muscles in the digestive system work.
How is functional constipation diagnosed according to Rome IV criteria?
According to the Rome IV criteria, functional constipation is diagnosed when a person experiences recurrent and chronic symptoms of constipation without any evidence of an underlying medical condition that can explain the symptoms.
To meet the diagnostic criteria for functional constipation, a person must experience at least two of the following symptoms for at least 3 months:
- Straining during bowel movements
- A feeling of incomplete evacuation after bowel movements
- Hard or lumpy stools
- Infrequent bowel movements (less than three per week)
Additionally, the person must not have any of the following criteria:
- Evidence of structural or biochemical abnormalities that would explain the symptoms
- Presence of irritable bowel syndrome (IBS)
- Evidence of inflammatory bowel disease (IBD), colon cancer, or other medical conditions that can cause constipation
Functional constipation is a common form of constipation and is often associated with lifestyle factors such as low fiber intake, inadequate hydration, lack of physical activity, and stress.
What are the symptoms of constipation?
The main symptom of constipation is difficulty passing stools or infrequent bowel movements. However, there are several other symptoms that may accompany constipation, including:
- Straining during bowel movements
- Feeling like you haven’t completely emptied your bowels after a bowel movement
- Hard or lumpy stools
- Abdominal pain or cramping
- Bloating
- Nausea
- Loss of appetite
- Feeling sluggish or tired
- Rectal bleeding or small tears in the anus (if you strain too hard)
When should I see a doctor for constipation?
Constipation is a common condition and can often be managed with lifestyle changes and over-the-counter treatments. However, there are some cases where it’s important to see a doctor for constipation. You should consider seeing a doctor if:
- Your constipation is severe or long-lasting: If you’ve been constipated for more than a few weeks, or if your constipation is causing significant discomfort, it’s important to see a doctor.
- You have blood in your stool: If you notice blood in your stool or on the toilet paper after wiping, it’s important to see a doctor to rule out any underlying conditions that may be causing the bleeding.
- You have abdominal pain or cramping: If you’re experiencing severe or persistent abdominal pain or cramping along with constipation, it’s important to see a doctor to rule out any underlying conditions that may be causing the pain.
- You have unintended weight loss: If you’re losing weight unintentionally and experiencing constipation, it’s important to see a doctor to rule out any underlying conditions that may be causing the weight loss.
- You have a family history of colon cancer: If you have a family history of colon cancer, it’s important to see a doctor for regular colon cancer screening, which may include checking for signs of constipation.
What tests may be done to evaluate constipation?
The tests that may be done to evaluate constipation depend on the underlying cause and severity of the symptoms. Some of the tests that healthcare providers may use to diagnose constipation or its underlying causes include:
- Physical examination: A healthcare provider may perform a physical examination to check for any abnormalities in the abdomen or rectum.
- Blood tests: Blood tests may be used to check for signs of infection, anemia, or other underlying conditions.
- Stool tests: Stool tests may be used to check for signs of infection, inflammation, or other abnormalities.
- Colonoscopy: A colonoscopy is a procedure in which a thin, flexible tube with a camera on the end is inserted into the rectum to examine the inside of the colon.
- Anorectal manometry: An anorectal manometry test measures the strength and coordination of the muscles in the anus and rectum.
- Transit studies: Transit studies involve tracking the movement of food and waste through the digestive system to identify any abnormalities.
The specific tests recommended will depend on the individual’s medical history, symptoms, and physical examination findings.
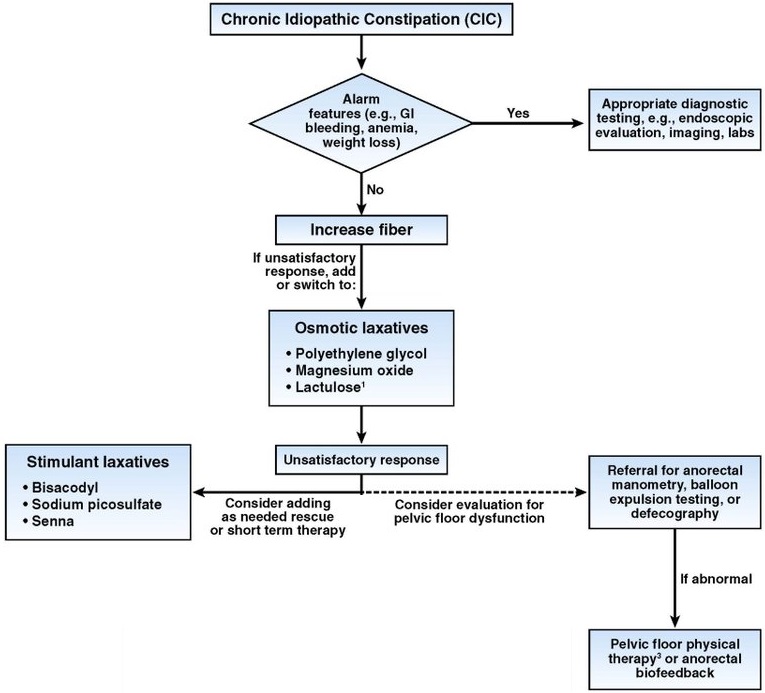
Chang L, et al. American Gastroenterological Association-American College of Gastroenterology Clinical Practice Guideline: Pharmacological Management of Chronic Idiopathic Constipation. Gastroenterology 2023;164:1086-1106.
What are the best over-the-counter laxatives for constipation?
There are several types of over-the-counter laxatives that can be used to treat constipation. The best type of laxative for you may depend on the severity of your constipation, your medical history, and other factors. Here are some of the most commonly used over-the-counter laxatives for constipation:
- Bulk-forming laxatives: These laxatives work by absorbing water in the intestines, which softens the stool and makes it easier to pass. Examples of bulk-forming laxatives include psyllium, methylcellulose, and polycarbophil.
- Stimulant laxatives: These laxatives work by stimulating the muscles in the intestines, which helps to move stool through the colon. Examples of stimulant laxatives include bisacodyl and senna.
- Osmotic laxatives: These laxatives work by drawing water into the intestines, which softens the stool and helps to move it through the colon. Examples of osmotic laxatives include magnesium hydroxide and polyethylene glycol.
- Lubricant laxatives: These laxatives work by coating the stool with a slippery substance, which makes it easier to pass. Examples of lubricant laxatives include mineral oil and glycerin suppositories.
It is important to follow the instructions on the package carefully when using over-the-counter laxatives, and to speak with a healthcare provider if you have any questions or concerns. Overuse of laxatives can lead to dependence and other health problems, so it is important to use them only as directed.
How to relieve constipation naturally?
There are several natural remedies that can help relieve constipation, including:
- Increase fiber intake: Eating a diet that is high in fiber can help promote regular bowel movements. Foods high in fiber include fruits, vegetables, whole grains, and legumes.
- Stay hydrated: Drinking plenty of water and other fluids can help keep stool soft and easier to pass. Aim to drink at least eight glasses of water a day.
- Exercise regularly: Regular physical activity can help stimulate bowel movements and improve digestion. Aim to get at least 30 minutes of moderate exercise most days of the week.
- Practice good bathroom habits: Try to establish a regular bathroom routine and take your time when using the toilet. Avoid delaying bowel movements when you feel the urge to go.
- Use natural laxatives: Certain foods can act as natural laxatives, including prunes, figs, and other dried fruits. Drinking warm liquids such as herbal tea or warm water with lemon can also help stimulate bowel movements.
- Try abdominal massage: Gentle massage of the abdomen can help stimulate bowel movements and relieve constipation. Start at the lower right side of the abdomen and use circular motions to massage the area.
How to treat constipation with diet?
Constipation can often be treated with dietary changes. Here are some ways to treat constipation with diet:
- Increase fiber intake: Eating a diet high in fiber can help promote regular bowel movements. Good sources of fiber include fruits, vegetables, whole grains, and legumes. Aim for at least 25-30 grams of fiber per day.
- Drink plenty of water: Staying hydrated can help keep your stool soft and easier to pass. Aim to drink at least eight glasses of water a day.
- Avoid foods that can cause constipation: Some foods can contribute to constipation, such as processed foods, red meat, and dairy products. Avoiding these foods or reducing your intake may help improve bowel regularity.
- Eat prunes or other high-fiber foods: Prunes are a natural laxative and can help stimulate bowel movements. Other high-fiber foods, such as figs, beans, and whole grains, can also help relieve constipation.
- Include probiotics in your diet: Probiotics are beneficial bacteria that can help improve digestion and promote regular bowel movements. Good sources of probiotics include yogurt, kefir, and fermented foods.
- Avoid or limit alcohol and caffeine: Alcohol and caffeine can contribute to dehydration, which can make constipation worse. Limit your intake of these substances or avoid them altogether.
What is a vibrating capsule for constipation?
A vibrating capsule for constipation is a medical device that is designed to stimulate bowel movements by delivering low-frequency vibrations to the colon. The capsule contains a small motor that generates vibrations, which are transmitted to the walls of the colon. The vibrations are intended to stimulate the muscles of the colon, causing it to contract and move waste material through the digestive tract.
Vibrating capsules are typically used in people who have chronic constipation that does not respond to other treatments, such as laxatives, dietary changes, or increased physical activity. The capsules are usually taken once a day, typically at bedtime, and can be used for up to two weeks at a time.
While vibrating capsules may be effective in some cases, they are not suitable for everyone. They may cause discomfort or side effects in some people, and they may not be effective in cases of severe or obstructive constipation.

What are the complications of chronic constipation?
Chronic constipation can lead to several complications, including:
- Hemorrhoids: Straining during bowel movements can put pressure on the veins in the rectum and anus, leading to the development of hemorrhoids.
- Anal fissures: Passing hard, dry stool can cause small tears in the lining of the anus, which can be painful and lead to bleeding.
- Fecal impaction: Chronic constipation can cause stool to become impacted in the colon, making it difficult or impossible to pass.
- Rectal prolapse: Chronic straining during bowel movements can weaken the muscles that support the rectum, leading to a condition called rectal prolapse, where the rectum protrudes from the anus.
- Bowel obstruction: In rare cases, chronic constipation can lead to a complete blockage of the colon, which requires emergency medical attention.
- Increased risk of colon cancer: Chronic constipation has been linked to an increased risk of colon cancer, although the exact mechanism is not fully understood.
Are there certain symptoms and sign that may indicate a more serious underlying condition?
While occasional constipation is common and usually not a cause for concern, there are certain signs and symptoms that may indicate a more serious underlying condition. These are known as “alarm signs” and include:
- Blood in the stool: If you notice blood in your stool or on toilet paper, it is important to speak with a healthcare provider right away, as this may be a sign of a more serious condition.
- Severe or persistent abdominal pain: Severe or persistent abdominal pain, especially if accompanied by vomiting or fever, may indicate a bowel obstruction or other serious condition.
- Changes in bowel habits: If you experience a sudden change in your bowel habits, such as a significant increase or decrease in frequency, it is important to speak with a healthcare provider.
- Unexplained weight loss: If you are experiencing unexplained weight loss, this may be a sign of a more serious underlying condition.
- Family history of colon cancer: If you have a family history of colon cancer, it is important to speak with a healthcare provider about recommended screening tests and other preventive measures.
If you are experiencing any of these alarm signs or symptoms, it is important to speak with a gastroenterologist right away.
How can I contact gastroenterologist Dr. Zavos for an appointment?
Dr. Chris Zavos is a board-certified gastroenterologist and hepatologist, located in Thessaloniki Greece, and specifically in Kalamaria suburb, about 7 kilometres (4 miles) southeast of downtown Thessaloniki. His private office is at: Fanariou 8 street (near Aigaiou and Adrianoupoleos avenues), Kalamaria (Thessaloniki), Greece.
Thessaloniki International Airport is only 10 km away from his private office in Kalamaria and can be reached by taxi within 13 minutes from the airport.
Dr. Chris Zavos performs endoscopies at Bioclinic private hospital in downtown Thessaloniki (Mitropoleos 86 street).
You can contact Dr. Zavos at phone numbers: (+30)-6976596988 and (+30)-2311283833, or you can email him at czavos@ymail.com. Dr. Zavos responds to Greek and English languages.
