What is Celiac Disease?
Celiac disease is a chronic autoimmune condition triggered by consuming gluten, a protein found in wheat, barley, and rye. When a person with celiac disease eats gluten, their immune system responds by damaging the villi of the small intestine, crucial for nutrient absorption. This disease differs from gluten intolerance, which causes discomfort without immune-mediated intestinal damage, and wheat allergy, a classic allergic reaction to wheat proteins.
What Causes Celiac Disease?
The exact cause is unknown, but it’s believed to result from a combination of genetic predisposition and environmental factors. Most people with celiac disease have one or both of the HLA-DQ2 or HLA-DQ8 genes. Environmental triggers may include gastrointestinal infections, pregnancy, surgery, or severe emotional stress. These factors can activate the disease in genetically susceptible individuals at any age.
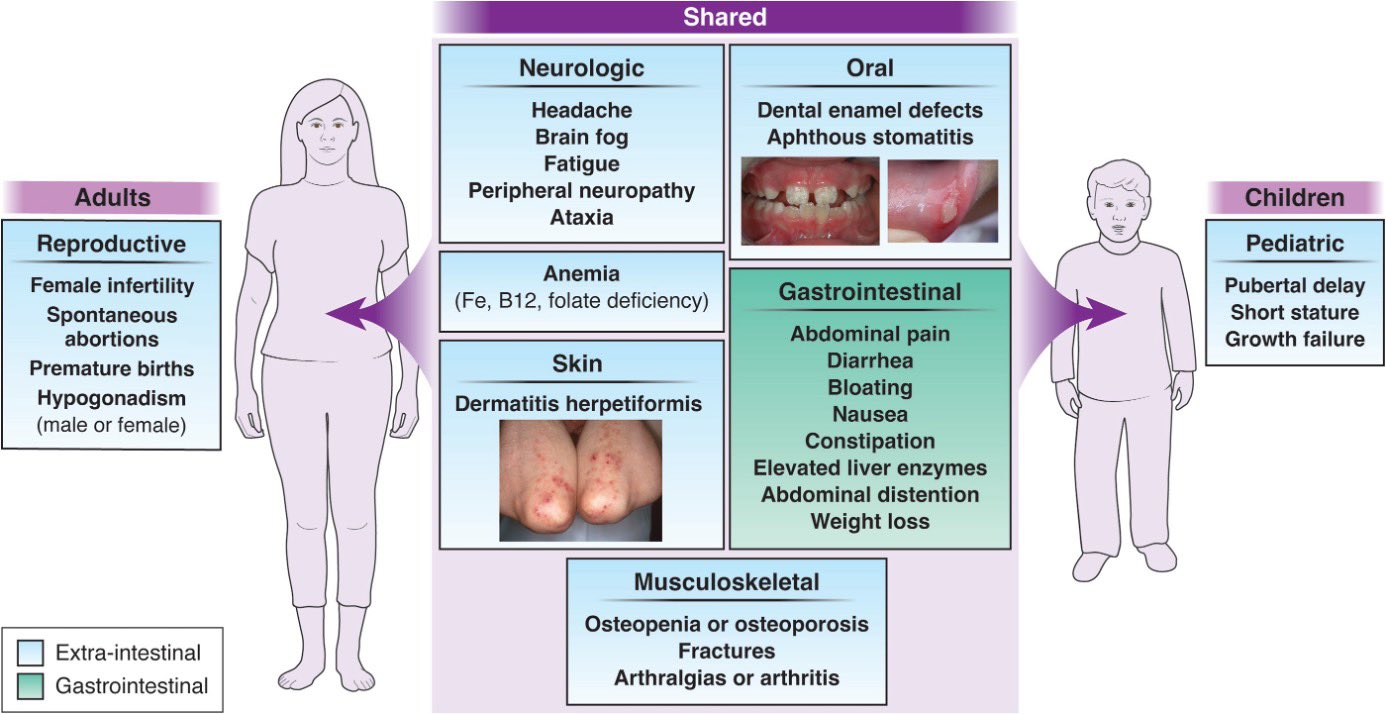
What are the Symptoms of Celiac Disease?
Symptoms vary greatly among individuals.
Classic symptoms include:
- chronic diarrhea
- abdominal pain
- bloating
- weight loss
In children, it may manifest as failure to thrive, delayed puberty, and dental enamel defects.
Atypical symptoms include:
- iron-deficiency anemia
- osteoporosis
- joint pain
- liver abnormalities
- migraine
- neurological issues
If left untreated, it can lead to serious complications like malnutrition, infertility, reduced bone density, neurological disorders, and an increased risk of certain cancers.
How is Celiac Disease Diagnosed?
The first step usually involves serology testing to look for elevated levels of certain autoantibodies. An endoscopy is then performed to take a biopsy from the small intestine to look for villous atrophy and inflammation, hallmark signs of celiac disease. Genetic testing can help rule out celiac disease if neither HLA-DQ2 nor HLA-DQ8 genes are present.
Can Celiac Disease be Cured?
Currently, there is no cure for celiac disease. The only effective treatment is a lifelong strict gluten-free diet. This diet allows the intestinal lining to heal and prevents further damage, leading to symptom relief and reduced risk of long-term complications.
What is a Gluten-Free Diet?
A gluten-free diet involves avoiding all foods that contain gluten. This includes most breads, pastas, cereals, and many processed foods. Gluten-free alternatives are made from corn, rice, quinoa, and other gluten-free grains. People with celiac disease should read food labels carefully, as gluten can be present in unexpected products like sauces, soups, and even some medications.
How to Live with Celiac Disease?
Living with celiac disease involves more than dietary changes. It requires education about the condition, reading food labels, and learning to identify hidden sources of gluten. Cross-contamination in kitchens where gluten-containing foods are prepared must be carefully managed. Support from healthcare providers, dietitians specializing in celiac disease, and patient support groups can be invaluable.
Can Celiac Disease Affect Other Parts of the Body?
Celiac disease can affect various body systems. Dermatitis herpetiformis is a itchy, blistering skin condition directly associated with gluten intake in celiac patients. It can also cause iron-deficiency anemia, reduced bone density (osteoporosis or osteopenia), fertility issues, and neurological complications like neuropathy and cognitive impairment.
Are There New Treatments on the Horizon?
Research into celiac disease is ongoing, focusing on understanding the disease mechanism and developing alternative therapies. These include drugs to degrade gluten in the stomach, prevent its absorption, or modulate the immune response. However, these are still in experimental stages and are not yet available as standard treatments.
Where to Find Support and Resources?
There are numerous resources for people with celiac disease. These include national celiac associations, which provide educational materials, guidance on diet management, and information on the latest research. Online forums and local support groups offer platforms to share experiences and coping strategies. You should also have a healthcare team experienced in managing celiac disease, including dietitians and gastroenterologists.
Bottom line
Understanding celiac disease, its management, and its impact on daily life is crucial for those diagnosed and their families. Ongoing research continues to improve our understanding and management of this condition.
