Evolving Strategies in Colorectal Cancer Prevention: A Focus on Polyp Surveillance
Colorectal cancer (CRC) remains a significant public health challenge, being the second leading cause of cancer death in the United States and Western Europe. Recent shifts in the prevention landscape have led to a better understanding of the role of polyp surveillance in reducing CRC incidence and mortality. However, the effectiveness of follow-up procedures post-polypectomy, particularly for nonadvanced polyps, remains a topic of ongoing debate and research.
The Impact of Screening and Detection
Screening has been proven to significantly reduce CRC incidence and mortality, especially when initiated for average-risk individuals. The detection and removal of polyps, which are potential precursors to CRC, play a central role in these prevention efforts. Despite the benefits of screening, the necessity and frequency of surveillance following the initial identification and removal of polyps are under scrutiny. The primary reason for this reevaluation is the low likelihood of polyp progression to CRC, given the lifetime risk remains between 3.9% and 4.3%.
Polyp Categorization and Surveillance Strategies
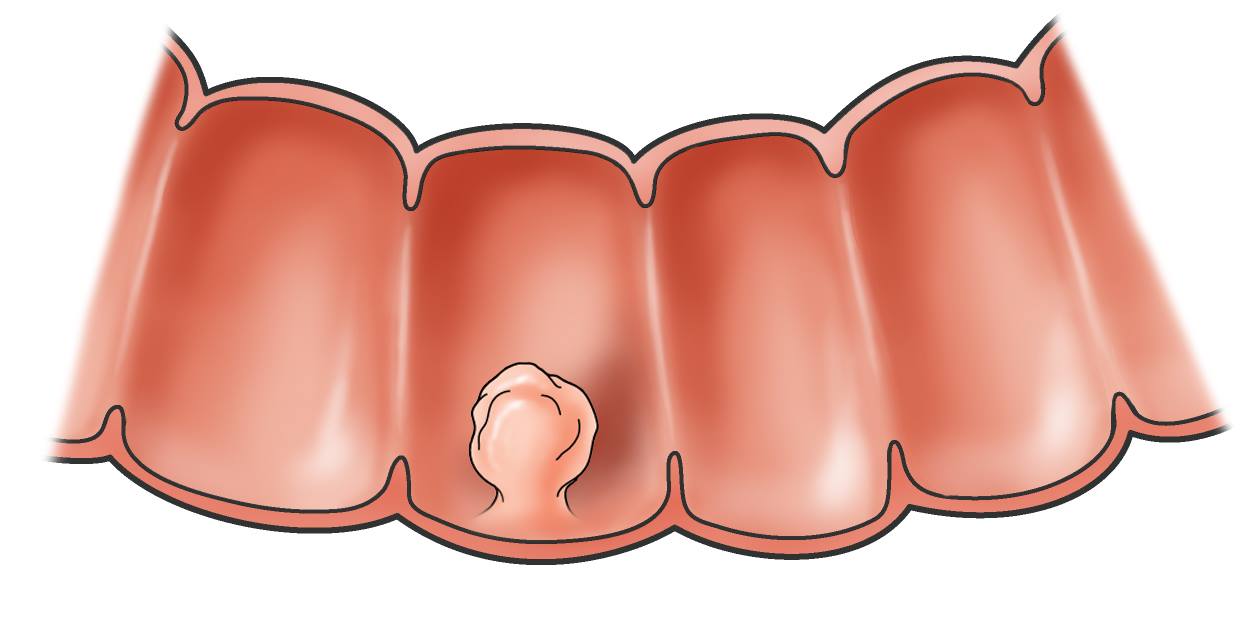
Polyps are commonly detected during CRC screenings, with prevalence rates ranging from 20% to over 50% in average-risk individuals. Advanced polyps, which include larger adenomas (≥10 mm), those with dysplasia, or villous histology, are found less frequently but are associated with a higher risk of developing CRC. In contrast, nonadvanced polyps, despite their higher detection rates, are associated with significantly lower future CRC risks.
U.S. guidelines, in contrast to some international protocols, emphasize more frequent surveillance of these polyps. This approach is driven by the ability to categorize polyps based on number, size, and histologic features which ostensibly indicate future CRC risk. However, the evidence increasingly suggests that individuals with one or two nonadvanced polyps might not require as stringent surveillance as those with advanced lesions due to their relatively lower CRC risk.
The frequency of polyp surveillance is a critical factor in the strategic management of colorectal cancer (CRC) prevention, influenced significantly by the type and characteristics of polyps detected during colonoscopy. For nonadvanced polyps, such as small tubular adenomas or sessile serrated lesions under 10 mm without high-risk histologic features, the evidence increasingly suggests that less frequent surveillance may be sufficient. This is based on findings that such polyps exhibit a much lower 10-year CRC risk, which might be comparable to the risk in the general population that undergoes regular screening. The current U.S. guidelines advocate for a more cautious approach, often suggesting surveillance intervals ranging from 5 to 10 years depending on the number and nature of these nonadvanced polyps, unless additional risk factors are present.
On the other hand, advanced polyps—defined as adenomas or SSLs that are 10 mm or larger, display villous features or high-grade dysplasia, or SSLs with any level of dysplasia—necessitate more frequent and rigorous surveillance. Individuals with these high-risk polyps are typically recommended to undergo follow-up colonoscopy at shorter intervals, commonly every 3 years, to closely monitor for any sign of recurrence or new polyp development. This heightened surveillance protocol is justified by the substantial increase in CRC risk associated with advanced polyps. The focus is to prevent the progression to CRC by early detection and management of any new or recurring neoplastic growths, reflecting a tailored approach to surveillance based on individual risk assessment and polyp pathology.
Epidemiological and Genetic Insights
The epidemiology of CRC underscores the importance of tailored prevention strategies. Risk factors such as age, gender, and lifestyle have well-established links with CRC incidence. Genetic research further enhances our understanding, identifying specific pathways from normal epithelium through adenoma stages to carcinoma, influenced by both genetic predispositions and environmental factors.
The age at which individuals begin colorectal cancer (CRC) screening and the frequency of subsequent surveillance is deeply influenced by risk factors and epidemiological data. Incidence rates for CRC rise with age, particularly after the age of 50, prompting recommendations for regular screening starting at age 45 to 50 in average-risk individuals. This age threshold was recently adjusted to 45 from 50 in the United States, reflecting a response to the rising incidence of CRC in younger populations. The decision to initiate screening at a younger age aims to capture and manage precancerous conditions like polyps before they progress to cancer, particularly in an era where lifestyle factors and genetic predispositions are leading to earlier disease onset. Surveillance intervals are then adjusted based on findings from the initial screening, with the goal of optimizing resource use and focusing preventive efforts where they are most likely to reduce mortality and morbidity from CRC.
Current Challenges and Research Directions
The rising incidence of detected polyps due to enhanced screening techniques and broader screening recommendations, including younger age groups, poses significant challenges. This increase necessitates a critical evaluation of surveillance protocols to ensure they are both effective and resource-efficient. The main questions revolve around the optimal timing of surveillance and the identification of individuals who would benefit most from follow-up interventions.
Conclusion
As the landscape of CRC prevention continues to evolve, it becomes crucial to integrate new epidemiological, genetic, and clinical data into existing protocols. Optimizing surveillance strategies based on risk stratification will not only improve outcomes but also enhance the cost-effectiveness of CRC prevention programs. The ongoing research aims to refine these strategies further, ensuring that surveillance and intervention are judiciously applied to those at genuine risk, thereby preserving health care resources and improving patient care.
Reference
- Sullivan BA, Lieberman DA. Colon Polyp Surveillance: Separating the Wheat From the Chaff. Gastroenterology 2024 May;166:743-757.