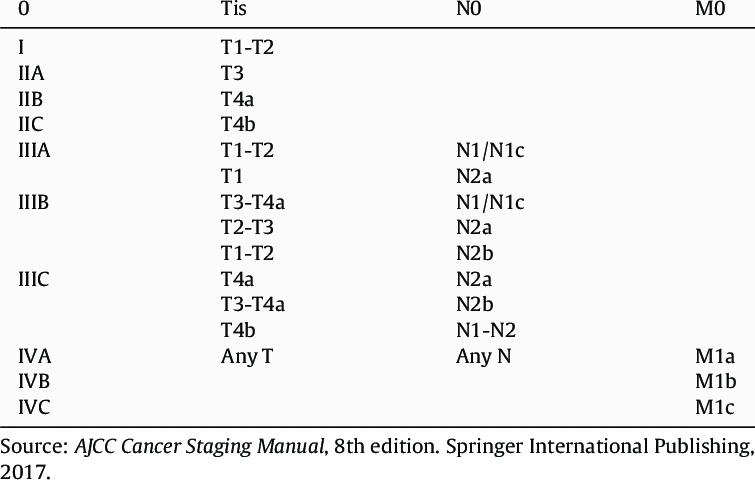
In the 8th edition of the American Joint Committee on Cancer (AJCC) staging manual, the section dedicated to colorectal cancer provides an extensive explanation of Tis dysplasia. Tis lesions, which penetrate into the lamina propria with the potential of invading the muscularis mucosa, are referred to as intramucosal adenocarcinoma. Invasive characteristics are attributed to penetration through the basement membrane at any gastrointestinal site. However, in colorectal cancer, only tumors that invade the submucosa have the ability to metastasize. Due to the possibility of sampling errors, Tis lesions are recorded in the cancer registry, while other forms of dysplasia, including high-grade, are not.
| AJCC Stage | Stage grouping | Description of colorectal cancer |
| 0 | Tis N0 M0 | The cancer is in its initial phase, often referred to as carcinoma in situ or intramucosal carcinoma (Tis). At this stage, it remains confined to the inner layer (mucosa) of the colon or rectum and has not extended further. |
| I | T1 or T2 N0 M0 | The cancer has progressed beyond the muscularis mucosa and invaded the submucosa (T1), and in some cases, it may have extended into the muscularis propria (T2). However, it has not metastasized to adjacent lymph nodes (N0) or distant locations (M0). |
| IIA | T3 N0 M0 | The cancer has infiltrated the outer layers of the colon or rectum without penetrating through them (T3). It has not extended to adjacent organs. Furthermore, it has not metastasized to nearby lymph nodes (N0) or distant locations (M0). |
| IIB | T4a N0 M0 | The cancer has breached the wall of the colon or rectum, but it has not infiltrated surrounding tissues or organs (T4a). At this stage, it has not metastasized to nearby lymph nodes (N0) or distant sites (M0). |
| IIC | T4b N0 M0 | The cancer has penetrated the wall of the colon or rectum and has either attached to or invaded adjacent tissues or organs (T4b). However, it has not metastasized to nearby lymph nodes (N0) or distant sites (M0) at this stage. |
|
IIIA
| T1 or T2 N1/N1c M0 | The cancer has advanced from the mucosa into the submucosa (T1), and there is a possibility that it has also invaded the muscularis propria (T2). Additionally, it has metastasized to a range of 1 to 3 nearby lymph nodes (N1) or to the fatty areas surrounding the lymph nodes but not the nodes themselves (N1c). However, it has not spread to distant locations (M0). |
| OR | ||
| T1 N2a M0 | The cancer has extended beyond the mucosa into the submucosa (T1). Additionally, it has metastasized to a range of 4 to 6 nearby lymph nodes (N2a). However, it has not spread to distant locations (M0). | |
|
IIIB
| T3 or T4a N1/N1c M0 | The cancer has infiltrated the outermost layers of the colon or rectum (T3) or even breached the visceral peritoneum (T4a), yet it has not involved nearby organs. Moreover, it has metastasized to a range of 1 to 3 nearby lymph nodes (N1a or N1b) or to the fatty areas surrounding the lymph nodes without affecting the nodes themselves (N1c). Importantly, it has not spread to distant locations (M0). |
| OR | ||
| T2 or T3 N2a M0 | The cancer has invaded the muscularis propria (T2) or progressed into the outer layers of the colon or rectum (T3). In addition, it has metastasized to a range of 4 to 6 nearby lymph nodes (N2a). However, it has not spread to distant locations (M0). | |
| OR | ||
| T1 or T2 N2b M0 | The cancer has advanced from the mucosa into the submucosa (T1), and there is a possibility that it has also infiltrated the muscularis propria (T2). Additionally, it has metastasized to 7 or more nearby lymph nodes (N2b). Importantly, it has not spread to distant locations (M0). | |
|
IIIC
| T4a N2a M0 | The cancer has extended beyond the wall of the colon or rectum, including the visceral peritoneum, but it has not invaded adjacent organs (T4a). Moreover, it has metastasized to a range of 4 to 6 nearby lymph nodes (N2a). Significantly, it has not spread to distant locations (M0). |
| OR | ||
| T3 or T4a N2b M0 | The cancer has infiltrated the outermost layers of the colon or rectum (T3) or even breached the visceral peritoneum (T4a), yet it has not extended to nearby organs. Furthermore, it has metastasized to 7 or more nearby lymph nodes (N2b). Importantly, it has not spread to distant locations (M0). | |
| OR | ||
| T4b N1 or N2 M0 | The cancer has penetrated the wall of the colon or rectum and has either attached to or invaded nearby tissues or organs (T4b). Moreover, it has metastasized to at least one nearby lymph node or infiltrated the fatty areas surrounding the lymph nodes (N1 or N2). Importantly, it has not spread to distant locations (M0). | |
| IVA | Any T Any N M1a | The cancer’s growth beyond the wall of the colon or rectum is present or absent (Any T). Its involvement with nearby lymph nodes is also present or absent (Any N). However, it has metastasized to a single distant organ, such as the liver or lung, or to a distant set of lymph nodes. Notably, it has not spread to distant areas of the peritoneum, which is the lining of the abdominal cavity (M1a). |
| IVB | Any T Any N M1b | The cancer’s infiltration through the wall of the colon or rectum and its involvement with nearby lymph nodes are present or absent (Any T, Any N). However, it has metastasized to multiple distant organs, such as the liver or lung, or to a distant set of lymph nodes. Importantly, it has not spread to distant regions of the peritoneum, which is the lining of the abdominal cavity (M1b). |
| IVC | Any T Any N M1c | The cancer’s penetration through the wall of the colon or rectum and its involvement with nearby lymph nodes are present or absent (Any T, Any N). However, it has disseminated to distant regions of the peritoneum, which is the lining of the abdominal cavity. Furthermore, it might or might not have extended to distant organs or lymph nodes (M1c). |
T4 is divided into T4a and T4b. T4a refers to tumors that invade the serosal surface (visceral peritoneum). It is further clarified that tumors with perforation, where the tumor cells are connected to the serosal surface through inflammation, are also categorized as T4a. However, T4a does not apply to areas of the colon and rectum without peritoneal covering, such as the posterior aspects of the ascending and descending colon and the lower rectum. Tumors that directly invade or adhere to adjacent organs or structures are classified as T4b.
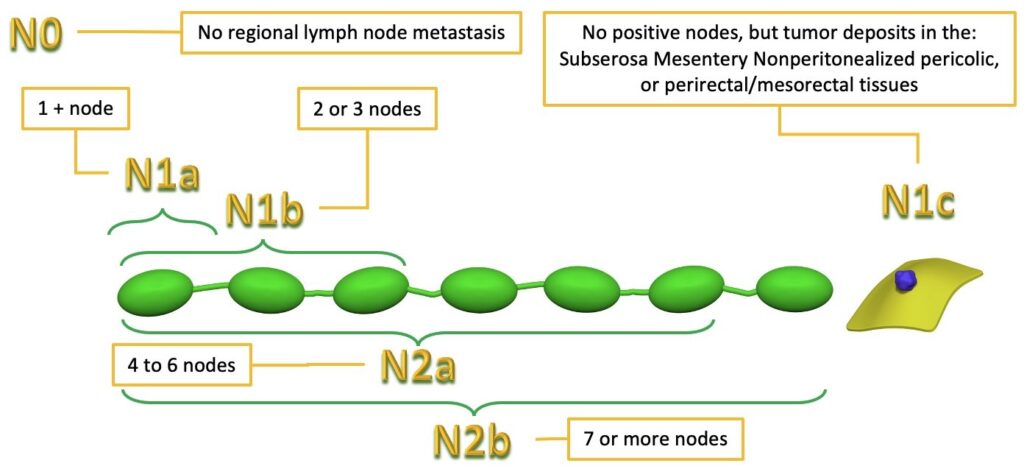
Isolated tumor cells typically consist of up to 20 cells within the subcapsular or marginal sinus of a lymph node and their prognostic value is subject to debate. They should be designated as N0 (or N0i+), but their presence does not elevate the disease to stage III. Micrometastases, on the other hand, are clusters of 20 or more cells or metastases measuring >0.2 mm and <2 mm in diameter. Recent meta-analyses have shown that micrometastases are associated with a poor prognosis. Lymph nodes containing micrometastases should be considered positive and denoted as N1.
Nodules without identifiable lymph node tissue or vascular/neural structures should be regarded as tumor deposits and designated as N1c. The shape, contour, and size of the deposit are not taken into consideration for these designations. Tumor deposits within a vessel wall should be considered as lymphovascular invasion, with the site-specific designations L+ for lymphatic or small-vein invasion and V+ for deposits in endothelial-cell-lined spaces accompanied by red blood cells or smooth muscle cells. Tumor nodules surrounding a neural structure should be categorized as perineural invasion.
The presence of N1c classifies the disease as stage III, even in the absence of nodal metastases. The number of tumor deposits is recorded with site-specific factors but does not impact the designation. In other words, a patient with one tumor deposit and a patient with four tumor deposits are both staged as N1c. The number of tumor deposits is not added to the number of positive lymph nodes.
The M category has been expanded with M1a denoting metastases to one distant site or organ, while M1b denoting metastases to multiple distant sites or organs. The addition of M1c designation in AJCC 8 reflects the understanding that patients with peritoneal metastases generally have a worse prognosis compared to those with metastases in visceral organs.
AJCC 8 provides a more comprehensive discussion of proper resection for colorectal cancer, including the measurement of the distance from the tumor to the circumferential margin, which is a site-specific factor, as well as the completeness of mesorectal excision. The four-point tumor regression grade introduced in AJCC 7 remains unchanged, and pathologic tumor response is reported with the prefix ‘y’ before pT and pN.
