Gastrointestinal Dysplasia: Understanding Causes, Types, Diagnosis, and Treatment
Gastrointestinal dysplasia refers to the abnormal growth and development of cells in the lining of the gastrointestinal (GI) tract. It is a precancerous condition that can occur in various parts of the GI tract, including the esophagus, stomach, small intestine, and colon. In this article, we will explore the causes, types, diagnosis, and treatment options for gastrointestinal dysplasia.
Causes of Gastrointestinal Dysplasia
The exact causes of gastrointestinal dysplasia are not fully understood, but several factors can contribute to its development. Some common causes include:
- Chronic Inflammation: Chronic inflammatory conditions, such as inflammatory bowel disease (Crohn’s disease or ulcerative colitis), can lead to persistent irritation and inflammation of the GI tract, increasing the risk of dysplasia.
- Barrett’s Esophagus: Barrett’s esophagus is a condition in which the lining of the lower esophagus is damaged by chronic acid reflux. This condition can progress to dysplasia and eventually esophageal cancer.
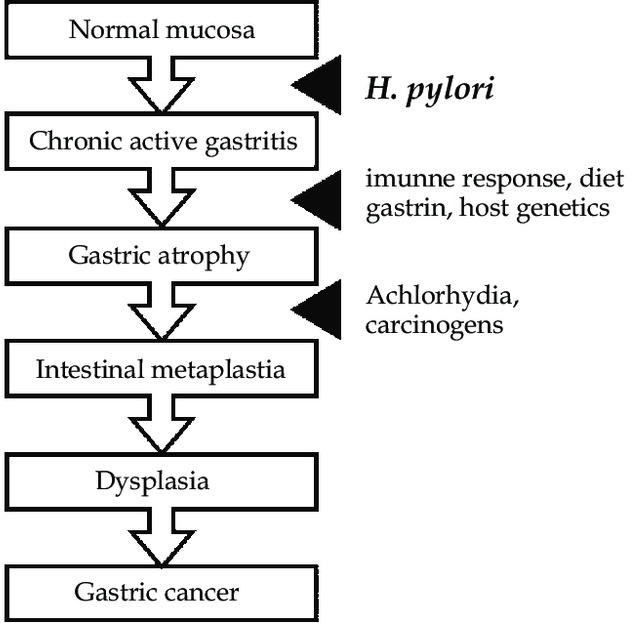
- Helicobacter pylori Infection: Chronic infection with the bacterium Helicobacter pylori, which is associated with gastritis and stomach ulcers, can lead to the development of dysplasia in the stomach. In the Figure below, you can see the model representing the role of Helicobacter pylori and other factors in gastric carcinogenesis, based on the cascade proposed by Correa.
- Hereditary Conditions: Certain hereditary conditions, such as familial adenomatous polyposis (FAP) and Lynch syndrome, increase the risk of developing gastrointestinal dysplasia.
Types of Gastrointestinal Dysplasia
Gastrointestinal dysplasia can manifest in different forms, depending on the location within the GI tract. Some common types include:
- Esophageal Dysplasia: Esophageal dysplasia occurs in the lining of the esophagus, often as a result of chronic acid reflux leading to Barrett’s esophagus. It is classified into low-grade and high-grade dysplasia, with the latter being more concerning and having a higher risk of progressing to esophageal cancer.
- Gastric Dysplasia: Gastric dysplasia refers to dysplastic changes in the lining of the stomach. It is often associated with Helicobacter pylori infection and can increase the risk of stomach cancer if left untreated.
- Colorectal Dysplasia: Colorectal dysplasia affects the lining of the colon and rectum. It is commonly seen in individuals with inflammatory bowel disease and can lead to the development of colorectal cancer.
Diagnosis of Gastrointestinal Dysplasia
The diagnosis of gastrointestinal dysplasia involves various methods to assess the extent and severity of dysplastic changes. The following diagnostic approaches are commonly used:
- Endoscopy: Endoscopic procedures, such as upper endoscopy or colonoscopy, allow direct visualization of the GI tract, enabling the collection of tissue samples for biopsy.
- Biopsy: During endoscopy, small tissue samples are collected from suspicious areas within the GI tract. These samples are then examined under a microscope to determine the presence and severity of dysplasia.
- Imaging Tests: Imaging techniques, such as CT scans or magnetic resonance imaging (MRI), may be used to assess the extent of dysplasia or detect any possible spread to nearby lymph nodes or organs.
Low grade vs. high grade dysplasia
- Low Grade Dysplasia: Low grade dysplasia refers to mild to moderate cellular changes that are considered less severe than high grade dysplasia. The cells in low grade dysplasia exhibit some abnormal characteristics but still retain some resemblance to normal cells. The abnormal cells may show increased cell division, changes in cell size and shape, and alterations in cell organization.
In the context of gastrointestinal dysplasia, such as in the esophagus, stomach, or colon, low grade dysplasia indicates that the cellular changes are relatively limited and have not fully acquired the features of invasive cancer. However, low grade dysplasia is still considered a precancerous condition because there is a higher risk of progressing to high grade dysplasia or invasive cancer over time.
- High Grade Dysplasia: High grade dysplasia represents a more advanced stage of abnormal cellular changes and is considered a more severe precancerous condition. In high grade dysplasia, the cells exhibit more pronounced and extensive abnormalities, often resembling cancer cells. The cellular changes in high grade dysplasia are closer to those seen in invasive cancer, but there is still a clear distinction between dysplastic cells and fully invasive cancer cells.
High grade dysplasia is associated with a higher risk of progression to invasive cancer compared to low grade dysplasia. Prompt intervention and treatment are typically recommended for high grade dysplasia to prevent the development of invasive cancer.
The classification and terminology of dysplasia may vary slightly depending on the organ or tissue involved. For instance, in the context of cervical dysplasia, the terms “CIN1” (mild dysplasia), “CIN2” (moderate dysplasia), and “CIN3” (severe dysplasia) are commonly used.
In summary, low grade dysplasia refers to mild to moderate cellular changes with less severe abnormalities, while high grade dysplasia represents more advanced and pronounced abnormal cellular changes, approaching the features of invasive cancer. Regular surveillance and appropriate management are essential for individuals diagnosed with dysplasia to prevent the progression to cancer.
Metaplasia vs. dysplasia
Metaplasia and dysplasia are both terms used to describe abnormal cellular changes in tissues, but they represent distinct processes and stages of cellular alteration. Understanding the difference between metaplasia and dysplasia is important in assessing tissue pathology and determining appropriate clinical management.
- Metaplasia: Metaplasia is a cellular adaptation process in which one mature cell type is replaced by another mature cell type. It occurs in response to chronic irritation, inflammation, or injury to a particular tissue. The transformation of one cell type to another is considered an adaptive response aimed at protecting the tissue from ongoing damage.
During metaplasia, the differentiated cells in a tissue are replaced by another type of specialized cells that are better suited to withstand the chronic stress or injury. This process involves reprogramming of stem cells or undifferentiated cells to differentiate into a different cell lineage. The new cell type is typically better able to tolerate the environmental changes and stressors.
For example, in the respiratory tract, chronic smoking can cause metaplastic changes in the normal ciliated columnar epithelium of the bronchi, leading to the replacement of these cells with stratified squamous epithelium. This metaplastic change is an adaptive response to protect the airways from the harmful effects of smoking, but it also increases the risk of developing dysplasia or cancer if the chronic exposure continues.
Metaplasia itself is not considered a precancerous condition, but it can increase the risk of subsequent dysplasia or neoplastic transformation if the underlying cause persists.
- Dysplasia: Dysplasia, on the other hand, refers to the abnormal growth and development of cells within a tissue. It represents a more advanced stage of cellular changes compared to metaplasia and is considered a precancerous condition. Dysplasia involves disordered cell growth, altered cell morphology, and abnormal cellular organization.
In dysplasia, cells display features such as increased nuclear size, nuclear pleomorphism (variation in size and shape), increased cell division, loss of normal tissue architecture, and disturbed cellular differentiation. These changes are indicative of cellular atypia and disruption of normal cell growth control mechanisms.
Dysplasia can occur in various tissues, including the epithelial linings of organs such as the cervix, esophagus, stomach, and colon. It is often detected through biopsy and microscopic examination. As mentioned earlier in this article, the severity of dysplasia is classified into low grade and high grade, with high grade dysplasia indicating more severe cellular abnormalities and a higher risk of progressing to invasive cancer.
Prompt diagnosis and treatment of dysplasia are crucial to prevent its progression to cancer. Treatment options may include surveillance, medication, endoscopic resection, surgical intervention, or ablative techniques, depending on the location and extent of dysplastic changes.
Treatment of Gastrointestinal Dysplasia
The treatment approach for gastrointestinal dysplasia depends on several factors, including the location, grade, and extent of dysplasia. The following treatment options may be considered:
- Surveillance: In cases of low-grade dysplasia or when the dysplastic changes are limited, close surveillance through regular endoscopic examinations (esophagogastroduodenoscopy and/or colonoscopy) and biopsies may be recommended. This allows for the monitoring of any progression or regression of dysplasia over time.
- Medications: Medications may be prescribed to manage underlying conditions that contribute to dysplasia, such as anti-inflammatory drugs for inflammatory bowel disease or antibiotics for Helicobacter pylori infection.
- Endoscopic Resection: For localized areas of dysplasia, endoscopic resection techniques, such as endoscopic mucosal resection (EMR) or endoscopic submucosal dissection (ESD), can be performed to remove the dysplastic tissue and reduce the risk of progression to cancer.
- Surgical Intervention: In cases of high-grade dysplasia or when dysplasia affects a larger area of the GI tract, surgical intervention may be necessary. This can involve the removal of the affected segment of the GI tract, such as esophagectomy or colectomy, to eliminate the dysplasia and reduce the risk of cancer development.
- Ablation Therapy: Ablation techniques, such as radiofrequency ablation (RFA) or photodynamic therapy (PDT), may be used to destroy dysplastic cells in the lining of the GI tract. These methods can be effective for treating Barrett’s esophagus or gastric dysplasia.
- Chemoprevention: Certain medications or supplements, such as aspirin, nonsteroidal anti-inflammatory drugs (NSAIDs), or specific antioxidants, may be used as chemopreventive agents to reduce the risk of dysplasia progression or the development of new dysplastic lesions.
Concluding remarks
Gastrointestinal dysplasia is a precancerous condition characterized by abnormal cell growth in the lining of the GI tract. It can occur in various parts of the digestive system and is associated with chronic inflammation, hereditary conditions, and certain infections. Early detection and management of gastrointestinal dysplasia are crucial to prevent its progression to cancer.
Regular surveillance, targeted treatments, and, in some cases, surgical interventions can effectively manage dysplasia and reduce the risk of developing gastrointestinal cancers. If you have concerns about gastrointestinal dysplasia, consult with a healthcare professional who can provide appropriate evaluation, diagnosis, and treatment options.
How can I contact gastroenterologist Dr. Zavos to arrange an appointment?
Dr. Chris Zavos is a board-certified gastroenterologist and hepatologist, located in Thessaloniki Greece, and specifically in Kalamaria suburb, about 7 kilometres (4 miles) southeast of downtown Thessaloniki. His private office is at: Fanariou 8 street (near Aigaiou and Adrianoupoleos avenues), Kalamaria (Thessaloniki), Greece.
Thessaloniki International Airport is only 10 km away from his private office in Kalamaria and can be reached by taxi within 13 minutes from the airport.
Dr. Chris Zavos performs endoscopies at Bioclinic private hospital in downtown Thessaloniki (Mitropoleos 86 street).
You can contact Dr. Zavos at phone numbers: (+30)-6976596988 and (+30)-2311283833, or you can email him at czavos@ymail.com. Dr. Zavos responds to Greek and English languages.
