Crohn’s Disease: A Chronic Inflammatory Intestinal Disease Affecting the Digestive System
Crohn’s disease is a chronic inflammatory bowel disease that affects the digestive system. It can impact both the upper and lower gastrointestinal tract. Crohn’s disease is characterized by inflammation that extends deeply into the layers of the affected intestinal wall.
Crohn’s disease can cause a range of symptoms, such as abdominal pain, diarrhea, and weight loss. It can also lead to complications like intestinal obstruction, abscesses, and fistulas. Crohn’s disease is believed to be caused by a combination of genetic and environmental factors. It is a lifelong condition with periods of flare-ups and remission, requiring ongoing management to control symptoms and prevent complications. In this article, you will find everything you would want to know about Crohn’s disease and its management.
What is Crohn’s Disease?
Crohn’s disease (also known as Crohn’s) was named after Dr. Burrill B. Crohn, who published the first relevant paper in 1932 along with his colleagues Gordon Oppenheimer and Leon Ginzburg.
Crohn’s disease belongs to the group of idiopathic inflammatory bowel diseases (including ulcerative colitis) and can cause diarrhea, abdominal pain, and other symptoms from the digestive system, which are further analyzed in this article.
No one knows exactly what causes Crohn’s disease. Also, no one can predict the course of the disease in a specific patient. Some patients may not experience symptoms for many years, while others may have frequent flare-ups. One thing is certain: Crohn’s disease is a chronic condition and is not completely curable.
Death from Crohn’s disease is very rare, but complications such as severe infections and colorectal cancer can occur. Despite a relatively increased risk of colorectal cancer compared to the general population, patients with Crohn’s disease overall have a very low risk, which increases 8-10 years after the diagnosis of Crohn’s disease. With regular monitoring through preventive colonoscopy, physical exercise, and a healthy diet, this risk is minimized, and Crohn’s disease is not fatal. Studies show that the life expectancy in patients with Crohn’s disease does not differ from that of the general population.
What Triggers Autoimmunity in Crohn’s Disease?
In healthy individuals, the body’s immune system kills microbes and “bad” cells that could turn into cancer. Sometimes, however, instead of killing only the “bad” cells, something goes wrong, and the immune system starts attacking healthy cells. This process is called an “autoimmune response” and leads to Crohn’s disease. In patients with Crohn’s disease, the immune system attacks the mucosa, the inner surface of the digestive system. This causes inflammation, which can lead to ulcers and bleeding. The symptoms of Crohn’s disease have periods of flare-ups and remission, but the disease is not curable. Fortunately, there are medications that improve the symptoms of the disease.
What Are the Symptoms of Crohn’s Disease?
Symptoms of Crohn’s disease include:
- Diarrhea
- Abdominal pain
- Fatigue
- Weight loss
- Fever
- Mouth ulcers
- Rashes
- Joint pain
- Redness in the eyes
- Fistulas and abscesses in the rectal area
Is There a Specific Test for Crohn’s Disease?
Yes. There are specific tests that can help diagnose Crohn’s disease. Gastroenterologists recommend radiographs or other imaging methods to examine the upper part of the intestine (small intestine) and colonoscopy to examine the lower part of the intestine (colon). During colonoscopy, the gastroenterologist inserts a thin flexible tube into the rectum and advances it to the cecum, the end point of the large intestine (lower right abdomen). The endoscope has a small camera connected to an external screen, allowing the gastroenterologist to see the lesions inside the intestine and take biopsies.
There are also markers in the blood and stool used in the diagnostic approach of patients with inflammatory bowel disease. The most important of these markers are C-reactive protein (CRP), fecal calprotectin, and fecal lactoferrin. The disadvantage of these markers is that they have varying sensitivity and specificity in diagnosing intestinal inflammation. Blood CRP has a low sensitivity of 0.49 and high specificity of 0.92. Fecal calprotectin has a sensitivity of 0.88 and a specificity of 0.73. Fecal lactoferrin has a sensitivity of 0.82 and a specificity of 0.79. Therefore, these three markers should be considered together, and of course, the confirmation of the disease should always be made with colonoscopy and based on the patient’s clinical picture.
What Can I Do to Feel Better from Crohn’s Disease?
If you have been diagnosed with Crohn’s disease, you can:
- Reduce foods that exacerbate your symptoms.
- Quit smoking, if you smoke. Smoking worsens symptoms and increases the chances of needing surgical intervention.
- Avoid drugs such as aspirin and non-steroidal anti-inflammatory drugs.
How is Crohn’s Disease Treated?
There are various medications that improve the symptoms of Crohn’s disease. These drugs reduce inflammation and the body’s immune response. Some drugs are administered during the flare-up of the disease, while others are administered as maintenance therapy to maintain disease remission. Antibiotics are sometimes prescribed to patients with Crohn’s disease but do not treat the disease itself.
During a flare-up of the disease, cortisone is usually administered, either orally or intravenously, in various forms (hydrocortisone, prednisone or prednisolone, methylprednisolone). A problem that gastroenterologists usually face is the equivalence of cortisone from one form to another. Calculate the mg of cortisone from one form to another automatically by clicking here.
My Gastroenterologist Suggested I Start a Biological Agent. What Is It and What Tests Will I Need to Do Beforehand?
Biological agents are substances that are normally produced in our body but for the treatment of inflammatory bowel diseases are produced industrially and administered intravenously or subcutaneously to patients who need them. Biological agents include specific antibodies against tumor necrosis factor-alpha (anti-TNF-α / infliximab or Remicade, adalimumab or Humira). There are also biosimilars of anti-TNF-α with the trade names Remsima and Inflectra.
In Crohn’s disease, a new biological agent against α4β7-integrin (vedolizumab, Entyvio) is also used. This agent is currently administered intravenously and is used either after failure of TNF-α therapy or as first-line therapy.
Also, the monoclonal antibody against interleukins 12 and 23 (anti-IL-12 & -23) marketed as Ustekinumab (STELARA) has been indicated. The induction phase of Crohn’s disease remission is done with intravenous administration, followed by the maintenance phase with subcutaneous administration of the drug. STELARA is indicated for the treatment of adult patients with moderately to severely active Crohn’s disease, who have shown an inadequate response, loss of response, or intolerance to conventional therapy or a TNF-α antagonist or have contraindications to these therapies.
Less commonly used biological agents in Crohn’s disease are Certolizumab pegol (Cimzia), which also inhibits TNF-α, and Natalizumab (Tysabri). Natalizumab is a selective inhibitor of adhesion molecules and binds to the α4 subunit of human integrins.
In July 2022, the biological agent Risankizumab (Skyrizi) received indication for moderate to severe Crohn’s disease. Risankizumab is a humanized monoclonal immunoglobulin G1 (IgG1) antibody that selectively binds with high affinity to the p19 subunit of human cytokine interleukin-23 (IL-23) and inhibits IL-23-dependent cellular signaling and release of pro-inflammatory cytokines.
The European Crohn’s and Colitis Organization (ECCO) has issued a list of necessary tests that every patient who is to be treated with a biological agent should undergo, regarding the management of infections.
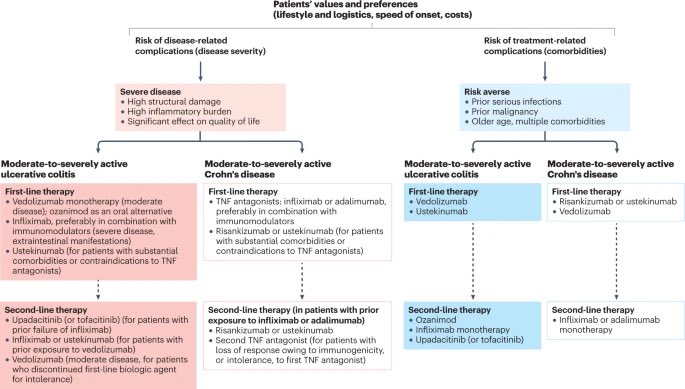
A useful algorithm for the use of biological agents in patients with IBD was published in 2023, and you can see it in the following Image (Singh S. Nat Rev Gastroenterol Hepatol 2023).
Is Surgery Necessary for Crohn’s Disease?
Surgery is necessary as a last resort if medications fail to control the symptoms of Crohn’s disease or if the medications cause severe side effects. Surgery does not cure the disease, but it can help you feel better and return to your daily activities.
The surgical intervention for the treatment of Crohn’s disease aims to:
- Remove the affected part of the colon.
- Restore the patency of the colon that has been obstructed.
Does Crohn’s Disease Increase the Risk of Developing Colorectal Cancer?
Possibly. The risk depends on the duration and extent of the disease. Experts recommend that patients with Crohn’s disease affecting the colon should be checked with colonoscopy at regular intervals, initially a few years after diagnosis and then once a year.
Does Crohn’s Disease Increase the Risk of Developing Genital Warts?
There is a 54% increased risk of developing genital warts in women with inflammatory bowel disease (33% increased risk regardless of gender), mainly in Crohn’s disease, according to a Danish study published in the journal of the European Gastroenterological Society in 2022. Patients need to be informed to get vaccinated for HPV. Systematic checks for genital warts, especially in women with Crohn’s disease receiving thiopurines as medication, should be conducted.
Is Crohn’s Disease Related to Irritable Bowel Syndrome?
According to a British study published in Alimentary Pharmacology & Therapeutics in August 2022, more than 2/3 of patients with inflammatory bowel disease suffer from irritable bowel syndrome. Irritable bowel syndrome in patients with inflammatory bowel disease is associated with increased hospitalization, increased risk of stress, depression, and somatoform disorders, and worse quality of life. However, irritable bowel syndrome does not negatively affect the course of inflammatory bowel disease.
Is Crohn’s Disease Related to Celiac Disease?
Patients with Crohn’s disease appear to have more than three times the risk of developing celiac disease compared to the general population (HR 3.31, 95%CI 2.69–4.06). The relevant study was published in September 2022 in the American Journal of Gastroenterology and included 48,551 patients with celiac disease and 83,529 patients with inflammatory bowel disease who were monitored for 20 years.
What Will My Life Be Like with Crohn’s Disease?
Patients with Crohn’s disease often need lifelong treatment. The majority of patients with Crohn’s disease live a fairly normal life.
I Have Crohn’s Disease. Can I Get Pregnant?
In most cases, Crohn’s disease does not affect a woman’s ability to get pregnant. If you want to get pregnant, talk to your gastroenterologist before you start trying to conceive. This will ensure that you have done all the necessary tests before and during your pregnancy. Medication modification may be required. This is because some of the drugs used to treat Crohn’s disease may not be safe for the embryo.
I’m Receiving Treatment for Crohn’s Disease and Have an Infection. Should I Stop the Treatment?
It depends on the type of infection (viral, bacterial, fungal, or Clostridium) and the type of treatment the patient is receiving for Crohn’s disease or ulcerative colitis (thiopurines, anti-TNF or anti-integrins).
References
- Zavos C, Kountouras J, et al. Targeting E-cadherin-catenin complex and eradicating Helicobacter pylori may be effective in managing inflammatory bowel disease and its complications. Med Hypotheses 2007 Mar;68(3):706-7.
- Kountouras J, Zavos C, et al. Low risk of colorectal cancer in a Greek cohort of inflammatory bowel disease patients. Aliment Pharmacol Ther 2014 May;39(9):1001-2.
- Terzoudis S, Zavos C, et al. The bone and fat connection in inflammatory bowel diseases. Inflamm Bowel Dis 2014; (in press)
- Kountouras J, Zavos C, et al. Autologous haematopoietic stem cell transplantation in a patient with refractory Crohn’s disease. J Crohns Colitis 2011 Jun;5(3):275-6.
- Terzoudis S, Zavos C, et al. Increased fracture risk assessed by Fracture Risk Assessment Tool in Greek patients with Crohn’s disease. Dig Dis Sci 2013 Jan;58(1):216-21.
- Kountouras J, Zavos C, et al. Apoptosis, inflammatory bowel disease and carcinogenesis: overview of international and Greek experiences. Can J Gastroenterol 2003 Apr;17(4):249-58.
- Kountouras J, Zavos C, et al. Apoptosis and apoptosis-related proteins in inflammatory bowel disease. Apoptosis 2004 Sep;9(5):657-8.
- Kountouras J, Zavos C, et al. Immunomodulatory benefits of cyclosporine A in inflammatory bowel disease. J Cell Mol Med 2004 Jul-Sep;8(3):317-28.
- Koutroubakis IE, Zavos C, et al. Role of ghrelin and insulin-like growth factor binding protein-3 in the development of osteoporosis in inflammatory bowel disease. J Clin Gastroenterol 2011 Jul;45(6):e60-5.
- Zavos C, Kountouras J, et al. Diagnostic role of upper gastrointestinal endoscopy in patients with inflammatory bowel disease. Ghana Med J 2007 Sep;41(3):144-5.
- Kapetanakis N, Zavos C, et al. Potential oncogenic properties of mobilized stem cells in a subpopulation of inflammatory bowel disease patients infected by Helicobacter pylori infection. Inflamm Bowel Dis 2013 Feb;19(2):E27-9.
- Elmahdi R, Thomsen LT, et al. Increased risk of genital warts in inflammatory bowel disease: A Danish registry-based cohort study (1996-2018). United European Gastroenterol J 2022 Mar 16.
- Fairbrass KM, Hamlin PJ, et al. Natural history and impact of irritable bowel syndrome-type symptoms in inflammatory bowel disease during 6 years of longitudinal follow-up. Aliment Pharmacol Ther 2022 Aug 22.
- Mårild K, Söderling J, et al. Association of Celiac Disease and Inflammatory Bowel Disease: A Nationwide Register-Based Cohort Study. Am J Gastroenterol 2022 Sep 1;117:1471-1481.
- Singh S. Positioning therapies for the management of inflammatory bowel disease. Nat Rev Gastroenterol Hepatol 2023
