Chios mastic gum in inflammatory bowel disease treatment
Background
Inflammatory bowel disease (IBD), encompassing Crohn’s disease (CD) and ulcerative colitis (UC), represents a group of intestinal disorders characterized by chronic inflammation of the gastrointestinal tract. The global prevalence of IBD underscores a significant health burden, with a noted increase in the incidence of colorectal cancer among affected individuals. Despite advances in understanding IBD’s multifactorial etiology—including genetic predisposition, immune dysregulation, and environmental factors—the complexity of its pathogenesis makes treatment challenging.
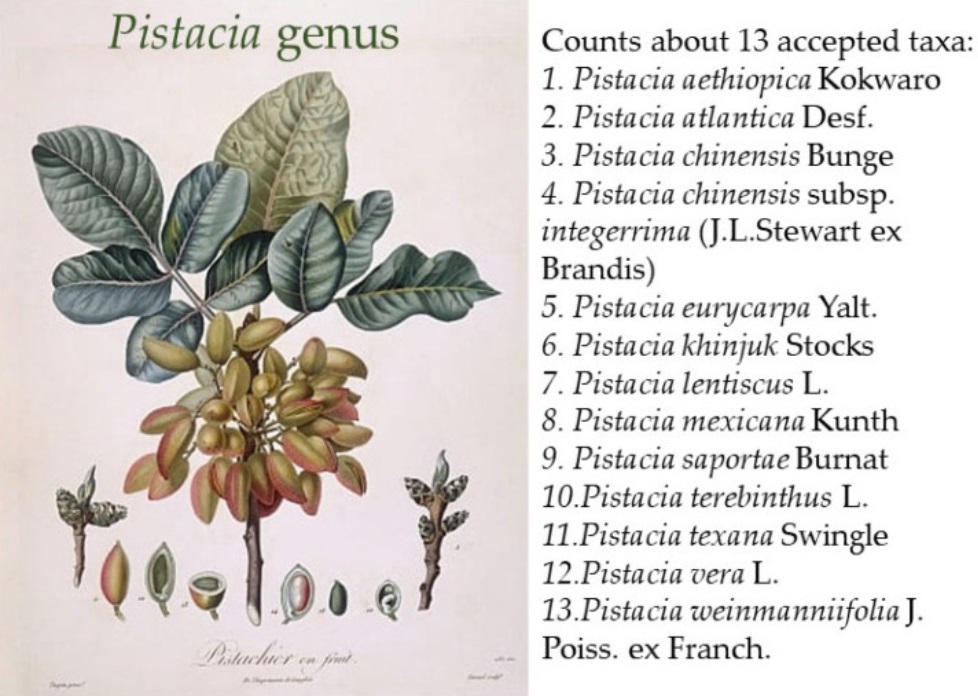
The potential of Pistacia lentiscus in IBD management
Recent explorations into complementary and traditional medicines have brought Pistacia lentiscus, particularly Chios mastic gum, into focus due to its unique effectiveness and moderate cost. Over 80% of the world’s population relies on traditional medicine systems, where herbal products play a pivotal role. Chios mastic gum, derived from Pistacia lentiscus, stands out for its potential in treating various gastrointestinal disorders through:
- Maintaining intestinal epithelial barrier integrity
- Regulating macrophage activation
- Modulating immune responses
- Inhibiting TNF-alpha activity
Scientific Evidence
Animal Models
Several studies utilizing animal models of IBD have demonstrated the anti-inflammatory effects of Pistacia lentiscus. These studies indicate that mastic gum can reduce the production of inflammatory cytokines such as TNF-α, IL-6, and IL-8, and promote histological improvement in colitis. Moreover, mastic gum’s components, particularly terpenes and phenolic compounds, are believed to scavenge free radicals and regulate key inflammatory mediators of IBD.
Clinical Trials
Clinical trials investigating the efficacy of Pistacia lentiscus, specifically mastic gum, in treating inflammatory bowel disease (IBD) provide critical insights into its potential therapeutic role. Although the body of evidence remains relatively small, these trials highlight mastic gum’s promise in managing IBD symptoms, improving patients’ quality of life, and possibly maintaining disease remission. Here’s a closer look at the notable clinical trials conducted to date:
1. Efficacy of Chios Mastic Gum on Active Crohn’s Disease
A pioneering study by Kaliora et al. in 2007 evaluated the effects of Chios mastic gum (CMG) on patients with active Crohn’s Disease (CD). Ten patients with mild to moderately active CD received mastic gum capsules (2.2 g/day) for four weeks. The trial observed significant reductions in the Crohn’s Disease Activity Index (CDAI) and inflammatory markers like C-reactive protein (CRP) and interleukin-6 (IL-6), leading to remission in seven out of ten patients. This study underscored CMG’s potential in regulating inflammation and oxidative stress in CD patients, suggesting its efficacy in inducing remission.
2. Impact on Quality of Life and Inflammatory Markers
Building on preliminary findings, Papada et al. conducted a randomized controlled trial in 2019 to explore CMG’s effects on IBD patients’ quality of life and inflammatory markers. Sixty eight patients with ulcerative colitis (UC) or Crohn’s disease (CD) were randomized to receive either CMG (2.8 g/day) or a placebo for three months, alongside their stable medical treatment. The CMG group showed a significant decrease in fecal lysozyme, an indicator of lower disease activity, and improvements in the Inflammatory Bowel Disease Questionnaire (IBDQ) scores, reflecting enhanced quality of life. These outcomes suggest CMG’s beneficial effects on disease activity and patients’ well-being.
3. Antioxidant Efficacy and Nutritional State Improvement
Another aspect of CMG’s potential therapeutic effects was explored in a study focusing on its antioxidant efficacy. Patients treated with CMG showed significant reductions in oxidized low-density lipoprotein (oxLDL) and improvements in plasma amino acids profiles, indicative of CMG’s antioxidant properties and its positive impact on the nutritional state of IBD patients.
4. Long-term Effects on Clinical Remission and Immunoregulatory Role
Further studies aimed to understand CMG’s long-term effects on clinical remission and its potential immunoregulatory role. A study by Amerikanou et al. investigated CMG’s regulatory effect on interleukin-17A (IL-17A) serum levels and alterations of the fecal metabolome in IBD patients. This trial found that CMG could modulate the gut microbiota composition, increase serum levels of beneficial amino acids, and potentially regulate Th17 cells’ function and differentiation, suggesting a role in maintaining remission and regulating immune responses.
Future Directions
Despite these encouraging results, the current body of clinical evidence on the effectiveness of mastic gum in IBD treatment remains limited, with most studies having small sample sizes and short duration. Future research should focus on larger, multicenter randomized controlled trials to fully assess CMG’s efficacy, optimal dosing, long-term safety, and its place in the therapeutic arsenal against IBD. These trials should aim to clarify CMG’s mechanism of action, its effects on different IBD phenotypes, and its impact on clinical outcomes to establish a robust evidence base for its use in clinical practice.
Conclusions
The literature on Pistacia lentiscus, particularly mastic gum, showcases its potential to reduce pro-inflammatory cytokines and improve the clinical course of IBD. Despite the promising data, the evidence from randomized controlled studies remains limited, and larger, more definitive trials are needed to fully ascertain Chios mastic gum’s therapeutic potential and efficacy in IBD treatment. The intriguing findings so far position mastic gum as a potential supplementary treatment to conventional IBD therapies, aiming to decrease disease activity, enhance nutritional status, and maintain clinical remission.
Also read:
- Chios mastic gum and Helicobacter pylori
- Pachi VK, Mikropoulou EV, Gkiouvetidis P, et al. Traditional uses, phytochemistry and pharmacology of Chios mastic gum (Pistacia lentiscus var. Chia, Anacardiaceae): A review. J Ethnopharmacol 2020 May 23;254:112485. doi: 10.1016/j.jep.2019.112485. Epub 2020 Feb 22. Erratum in: J Ethnopharmacol 2021;273:113961.
- Papalois A, Gioxari A, Kaliora AC, et al. Chios mastic fractions in experimental colitis: implication of the nuclear factor κB pathway in cultured HT29 cells. J Med Food 2012;15:974-83.
- Kaliora AC, Stathopoulou MG, Triantafillidis JK, et al. Chios mastic treatment of patients with active Crohn’s disease. World J Gastroenterol 2007;13:748-53.
- Papada E, Gioxari A, Amerikanou C, et al. Regulation of faecal biomarkers in inflammatory bowel disease patients treated with oral mastiha (Pistacia lentiscus) supplement: A double-blind and placebo-controlled randomised trial. Phytother Res 2019;33:360-369.
- Amerikanou C, Dimitropoulou E, Gioxari A, et al. Linking the IL-17A immune response with NMR-based faecal metabolic profile in IBD patients treated with Mastiha. Biomed Pharmacother 2021;138:111535.