What is gastroesophageal reflux disease (GERD), and what causes it?
Gastroesophageal reflux disease (GERD) is a chronic digestive disorder that occurs when the stomach acid or stomach contents flow back into the esophagus. This happens when the lower esophageal sphincter (LES) – a circular band of muscle that connects the esophagus to the stomach – does not close properly, allowing stomach acid to leak into the esophagus.
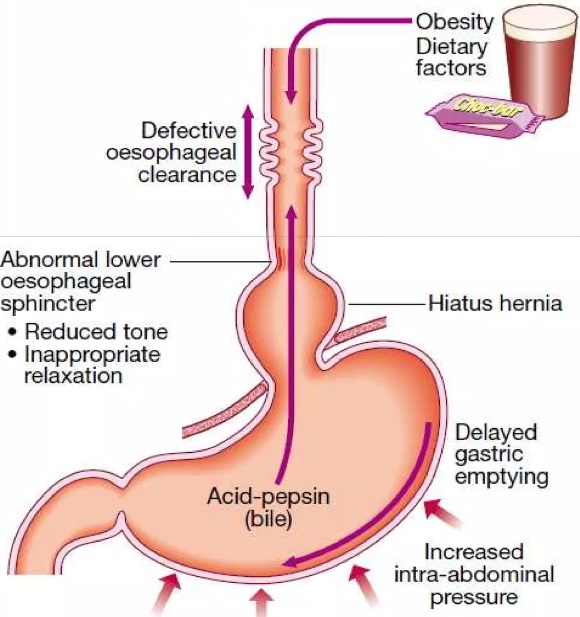
The exact cause of GERD is not always clear, but several factors can contribute to the development of the condition, including:
- Abnormalities in the LES: The LES may become weakened or relax inappropriately, allowing stomach acid to reflux into the esophagus.
- Hiatal hernia: This occurs when a portion of the stomach protrudes upward through the diaphragm into the chest cavity, which can weaken the LES and contribute to GERD.
- Delayed stomach emptying: When the stomach does not empty properly, the contents can back up into the esophagus, causing reflux.
- Obesity: Excess weight can increase pressure on the abdomen, which can push stomach contents back into the esophagus.
- Certain foods and beverages: Certain foods and drinks, such as fatty or spicy foods, citrus fruits, tomatoes, and alcohol, can trigger GERD symptoms.
- Smoking: Smoking can weaken the LES and contribute to GERD.
- Pregnancy: Hormonal changes and pressure on the abdomen during pregnancy can increase the risk of GERD.
- Medications: Certain medications, such as aspirin, ibuprofen, and certain muscle relaxers, can contribute to GERD.
Overall, GERD is a complex condition with multiple contributing factors. It is important to work with a gastroenterologist to identify and address these factors to effectively manage GERD symptoms.
What are the symptoms of gastroesophageal reflux disease (GERD)?
The symptoms of GERD can vary from person to person, but some of the most common symptoms include:
- Heartburn: A burning sensation in the chest that often occurs after eating, especially when lying down or bending over.
- Regurgitation: The sensation of acid or food coming back up into the throat or mouth.
- Difficulty swallowing: Some people with GERD may experience difficulty swallowing, also known as dysphagia.
- Chest pain: GERD can cause chest pain that may be mistaken for a heart attack, particularly in people who experience severe or frequent symptoms.
- Chronic cough: GERD can cause a chronic cough that does not respond to traditional cough treatments.
- Hoarseness: GERD can cause chronic hoarseness or a change in voice.
How is gastroesophageal reflux disease (GERD) diagnosed?
Your provider may recommend diagnostic tests to confirm the diagnosis of GERD and to rule out other conditions with similar symptoms. Some of the most common tests used to diagnose GERD include:
- Esophagogastroduodenoscopy: This procedure involves inserting a flexible tube with a camera (endoscope) down the throat and into the esophagus and stomach to look for signs of inflammation or damage.
- Esophageal pH monitoring: This test measures the amount of acid in the esophagus over a 24-hour period and can help diagnose GERD and evaluate the effectiveness of treatment.
- Barium swallow: This test involves drinking a liquid containing barium, which coats the lining of the esophagus and stomach, allowing X-rays to be taken to look for signs of reflux.
How is gastroesophageal reflux disease (GERD) treated, and what lifestyle modifications can I make to manage my symptoms?
The treatment of GERD typically involves a combination of lifestyle modifications, medications, and in some cases, surgery. The goal of treatment is to relieve symptoms, reduce the frequency and severity of reflux episodes, and prevent complications such as esophageal inflammation, ulcers, and strictures. Here are some common treatment options:
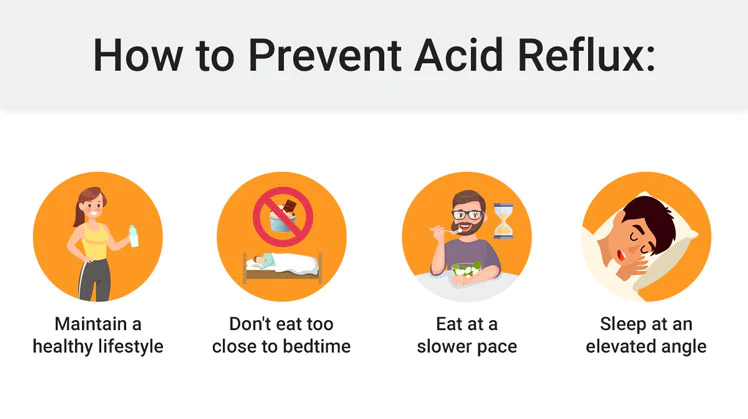
- Lifestyle modifications: Certain changes to your diet and lifestyle can help alleviate GERD symptoms. These include:
- Eating smaller, more frequent meals
- Avoiding trigger foods that can worsen symptoms, such as fatty or spicy foods, caffeine, alcohol, and chocolate
- Avoiding lying down or bending over after meals
- Elevating the head of your bed to prevent nighttime reflux
- Losing weight if you are overweight or obese
- Quitting smoking
- Medications: Several types of medications can be used to treat GERD, including:
- Antacids: These over-the-counter medications can neutralize stomach acid and provide temporary relief from symptoms.
- H2 blockers: These medications reduce the amount of acid your stomach produces and can provide longer-lasting relief than antacids.
- Proton pump inhibitors (PPIs): These medications are highly effective at reducing acid production and are typically used for more severe or chronic cases of GERD.
- Prokinetics: These medications help strengthen the lower esophageal sphincter (LES) and promote gastric emptying, which can reduce the frequency and severity of reflux episodes.
- Chios mastic gum. See relevant article on peptiko.gr
- Surgery: In some cases, surgery may be necessary to treat GERD. The most common procedure is called fundoplication, which involves wrapping the upper part of the stomach around the lower esophagus to create a new LES that prevents reflux.
- Endoscopic treatments: Newer minimally invasive endoscopic treatments have also been developed in recent years, such as radiofrequency ablation (RFA), transoral incisionless fundoplication (TIF), and magnetic sphincter augmentation (LINX). These treatments use advanced technology to improve the function of the LES and reduce symptoms of GERD.
In addition to these treatment options, there are several lifestyle modifications you can make to help manage your GERD symptoms, such as:
- Maintaining a healthy weight
- Avoiding tight-fitting clothing
- Practicing stress-reduction techniques such as yoga or meditation
- Eating a diet rich in fiber and whole grains
- Drinking plenty of water
- Chewing gum or sucking on hard candy to stimulate saliva production, which can help neutralize acid in the esophagus
Can gastroesophageal reflux disease (GERD) lead to other complications, such as Barrett’s esophagus or esophageal cancer?
Yes, gastroesophageal reflux disease (GERD) can lead to other complications, including Barrett’s esophagus and esophageal cancer. Barrett’s esophagus is a condition in which the normal lining of the esophagus is replaced with abnormal cells, which can increase the risk of developing esophageal cancer.
Chronic acid reflux from GERD can irritate and damage the lining of the esophagus over time, which can lead to the development of Barrett’s esophagus. People with Barrett’s esophagus have a higher risk of developing esophageal cancer than people without the condition.
Esophageal cancer is a rare but serious complication of GERD. Over time, the chronic inflammation and damage to the lining of the esophagus can increase the risk of developing cancerous cells.
Not everyone with GERD will develop Barrett’s esophagus or esophageal cancer, and the risk factors for developing these complications are not fully understood.
How often do I need to follow up with my healthcare provider for gastroesophageal reflux disease (GERD) management?
The frequency of follow-up appointments for gastroesophageal reflux disease (GERD) management can vary depending on the severity of your symptoms and the effectiveness of your treatment plan. In general, it is recommended to have regular follow-up appointments with your healthcare provider to monitor your symptoms, adjust your treatment plan as needed, and address any concerns or questions you may have.
For people with mild to moderate GERD symptoms, follow-up appointments may be scheduled every few months to monitor symptoms and adjust treatment as needed. For people with more severe symptoms or complications such as Barrett’s esophagus or esophageal cancer, more frequent follow-up appointments may be necessary.
Are there any dietary restrictions or changes I should make to manage my gastroesophageal reflux disease (GERD) symptoms?
Yes, making dietary changes is an important part of managing gastroesophageal reflux disease (GERD) symptoms. Here are some dietary tips that may help reduce your symptoms:
- Avoid Trigger Foods: Certain foods and drinks can trigger GERD symptoms, such as spicy and fatty foods, citrus fruits and juices, tomato-based products, chocolate, caffeine, and alcohol. Try to avoid these foods or limit their intake.
- Eat Smaller Meals: Eating large meals can put pressure on the stomach and worsen GERD symptoms. Instead, eat smaller meals throughout the day.
- Avoid Eating Late at Night: Eating close to bedtime can increase the risk of GERD symptoms, especially if you lie down right after eating. Try to eat at least 2-3 hours before bedtime.
- Stay Upright After Eating: Lying down after eating can worsen GERD symptoms. Try to stay upright for at least 3 hours after eating.
- Chew Your Food Thoroughly: Eating too quickly or not chewing your food well can increase the risk of GERD symptoms. Chew your food thoroughly to aid digestion.
- Elevate Your Head While Sleeping: Elevating your head while sleeping can help reduce GERD symptoms at night. Use a wedge pillow or elevate the head of your bed by 6-8 inches.
- Stay Hydrated: Drink plenty of water to help dilute stomach acid and reduce the risk of GERD symptoms.
Does stress cause gastroesophageal reflux disease (GERD)?
Stress can worsen gastroesophageal reflux disease (GERD) symptoms, but it is not a direct cause of GERD. However, stress can lead to behaviors that increase the risk of developing GERD or make existing symptoms worse, such as overeating, smoking, and consuming alcohol or caffeine.
Stress can also cause physical changes in the body that can contribute to GERD symptoms. For example, stress can increase the production of stomach acid, weaken the lower esophageal sphincter (the muscle that separates the esophagus from the stomach), and delay gastric emptying, which can all worsen GERD symptoms.
If you are experiencing stress-related GERD symptoms, it is important to find ways to manage stress, such as through relaxation techniques like deep breathing, meditation, or yoga, regular exercise, and getting enough sleep. It is also important to follow a healthy diet and lifestyle habits, and to work with your gastroenterologist to develop a treatment plan that meets your individual needs.
Can gastroesophageal reflux disease (GERD) cause arrhythmias?
While GERD itself does not directly cause arrhythmias, there are several ways in which GERD can indirectly contribute to arrhythmias. One possible way is through the stimulation of the vagus nerve, which runs from the brainstem to the abdomen and helps regulate various bodily functions, including heart rate. Acid reflux can irritate the vagus nerve, causing it to release neurotransmitters that can slow down the heart rate and potentially cause arrhythmias.
In addition, GERD can lead to electrolyte imbalances in the body, particularly low levels of potassium and magnesium, which can disrupt the normal electrical activity of the heart and increase the risk of arrhythmias.
Furthermore, certain medications used to treat GERD, such as proton pump inhibitors and H2 blockers, can interact with other medications that affect heart rate and rhythm, potentially increasing the risk of arrhythmias.
While GERD can contribute to arrhythmias, the risk is generally low and most people with GERD do not experience any cardiac complications.
Is irritable bowel syndrome (IBS) associated with gastroesophageal reflux disease (GERD)?
Irritable bowel syndrome (IBS) and gastroesophageal reflux disease (GERD) are both gastrointestinal conditions, but they affect different parts of the digestive system and are not directly associated with each other.
IBS is a chronic condition characterized by a group of symptoms that may include abdominal pain, bloating, constipation, diarrhea, or alternating bouts of constipation and diarrhea. The cause of IBS is not fully understood, but it is thought to be related to a combination of factors, including genetics, gut bacteria, and abnormal intestinal motility.
On the other hand, GERD is a condition in which stomach acid flows back up into the esophagus, causing symptoms such as heartburn, chest pain, and difficulty swallowing. It is caused by a weakened lower esophageal sphincter (LES), which allows stomach acid to enter the esophagus.
While IBS and GERD are not directly associated with each other, some people with IBS may also experience symptoms of GERD, such as heartburn or acid reflux. This may be due to the fact that both conditions can be exacerbated by certain dietary factors, such as spicy or fatty foods, caffeine, or alcohol.
Additionally, some medications used to treat IBS, such as antidepressants or muscle relaxants, can also relax the LES and increase the risk of GERD symptoms.
Does pregnancy exacerbate gastroesophageal reflux disease (GERD)?
Yes, pregnancy can exacerbate gastroesophageal reflux disease (GERD). The hormonal changes that occur during pregnancy, particularly the increase in progesterone levels, can relax the lower esophageal sphincter (LES), the muscle that separates the esophagus from the stomach. This can allow stomach acid to reflux back into the esophagus, causing heartburn, acid reflux, and other GERD symptoms.
In addition to hormonal changes, the physical changes that occur during pregnancy can also contribute to GERD symptoms. As the uterus expands, it can push the stomach upward and increase pressure on the LES, making it more likely to allow stomach acid to reflux into the esophagus.
Furthermore, as the pregnancy progresses and the baby grows, the pressure on the stomach can also increase, further exacerbating GERD symptoms.
While GERD is common during pregnancy, there are several steps that can be taken to manage symptoms, such as avoiding trigger foods, eating smaller meals more frequently, and avoiding lying down after eating. In some cases, medications may also be prescribed to help manage symptoms.
Do asthma and gastroesophageal reflux disease (GERD) occur together?
Yes, asthma and gastroesophageal reflux disease (GERD) often occur together. Studies have shown that up to 80% of people with asthma also have GERD, and vice versa. While the exact relationship between the two conditions is not fully understood, there are several theories as to why they may be related.
One theory is that the acid reflux that occurs with GERD can irritate the airways and trigger asthma symptoms. Acid reflux can cause inflammation and narrowing of the airways, which can make it harder to breathe and trigger asthma symptoms such as wheezing, coughing, and shortness of breath.
Another theory is that asthma medications, particularly bronchodilators, can relax the lower esophageal sphincter (LES), the muscle that separates the esophagus from the stomach, making it more likely that stomach acid will reflux into the esophagus and trigger GERD symptoms.
Regardless of the exact mechanism, people with both asthma and GERD should receive appropriate treatment for both conditions in order to effectively manage symptoms. This may involve medications to manage asthma symptoms, such as inhalers or oral medications, as well as lifestyle modifications to manage GERD symptoms, such as avoiding trigger foods, eating smaller meals more frequently, and avoiding lying down after eating. In some cases, surgery may also be recommended to repair the LES and prevent acid reflux.
Does insomnia affect gastroesophageal reflux disease (GERD)?
Yes, insomnia can affect gastroesophageal reflux disease (GERD) and may even worsen GERD symptoms. Insomnia refers to difficulty falling asleep or staying asleep, and it can be caused by a variety of factors, including stress, anxiety, depression, and certain medications.
Studies have shown that people with GERD are more likely to experience insomnia than people without GERD, and that insomnia can in turn worsen GERD symptoms. One reason for this may be that lying down flat can increase the likelihood of acid reflux, and people with insomnia may be more likely to lie awake in bed for extended periods of time, increasing their risk of acid reflux.
Furthermore, the stress and anxiety associated with insomnia can also worsen GERD symptoms. Stress and anxiety can cause the body to produce more stomach acid, which can exacerbate GERD symptoms such as heartburn and acid reflux.
Treatment plan for both conditions may involve medications to manage GERD symptoms, as well as cognitive-behavioral therapy (CBT) or other behavioral interventions to manage insomnia. Making lifestyle modifications, such as avoiding trigger foods, eating smaller meals more frequently, and avoiding lying down after eating, may also help to improve both GERD symptoms and insomnia.
What is the difference between laryngopharyngeal reflux disease (LPRD) and gastroesophageal reflux disease (GERD)?
Laryngopharyngeal reflux disease (LPRD) and gastroesophageal reflux disease (GERD) are two related conditions that involve the reflux of stomach acid into the upper gastrointestinal tract. However, they differ in terms of the specific symptoms and anatomical locations affected.
GERD primarily involves the reflux of stomach acid into the lower esophagus, causing symptoms such as heartburn, regurgitation, and chest pain. The lower esophageal sphincter, a muscular ring that normally acts as a barrier between the esophagus and the stomach, may be weakened or dysfunctional in people with GERD, allowing acid to flow back into the esophagus.
LPRD, on the other hand, involves the reflux of stomach acid into the upper airway, including the larynx (voice box) and pharynx (throat). Symptoms of LPRD may include hoarseness, chronic cough, throat clearing, a sensation of something stuck in the throat, and difficulty swallowing. Unlike GERD, LPRD may not cause classic heartburn symptoms, making it more difficult to diagnose.
While both GERD and LPRD involve the reflux of stomach acid, the causes and risk factors for the two conditions may differ. For example, obesity, smoking, and alcohol consumption may be more strongly associated with GERD, while factors such as voice use, poor sleep habits, and certain medications may be more strongly associated with LPRD.
Treatment for GERD and LPRD may also differ depending on the specific symptoms and underlying causes. While lifestyle modifications such as avoiding trigger foods and elevating the head of the bed may be helpful for both conditions, medications such as proton pump inhibitors (PPIs) or H2 blockers may be more effective for GERD, while voice therapy or other behavioral interventions may be more effective for LPRD.
Are home remedies for gastroesophageal reflux disease (GERD) effective?
While home remedies can be helpful in managing mild symptoms of gastroesophageal reflux disease (GERD), they also have several potential disadvantages that should be taken into consideration:
- Limited effectiveness: Home remedies may not provide complete relief from GERD symptoms, especially in severe cases. They may also take longer to work than medications or other treatments.
- Delayed diagnosis: Relying on home remedies may delay the diagnosis of a more serious condition, such as Barrett’s esophagus or esophageal cancer. These conditions may have similar symptoms to GERD but require medical intervention.
- Masking symptoms: Home remedies may mask symptoms of GERD without addressing the underlying cause, such as a hiatal hernia or weak lower esophageal sphincter. This can lead to the progression of the disease and potentially more serious complications.
- Interference with medical treatment: Some home remedies may interfere with medical treatment for GERD, such as by reducing the effectiveness of medications or increasing the risk of side effects.
- Risk of side effects: Some home remedies may have side effects, particularly if used in excess or by people with certain medical conditions. For example, consuming large amounts of baking soda can lead to electrolyte imbalances, while apple cider vinegar can erode tooth enamel and irritate the throat.
In summary, while home remedies can be helpful in managing GERD symptoms, they should not be relied upon as the sole form of treatment.
Is gastroesophageal reflux disease (GERD) hereditary?
There is evidence to suggest that genetics may play a role in the development of gastroesophageal reflux disease (GERD), although the exact genetic factors involved are not fully understood.
Studies have found that a family history of GERD is associated with an increased risk of developing the condition. For example, one study found that individuals with a first-degree relative (parent, sibling, or child) with GERD had a 1.4-fold increased risk of developing the condition themselves compared to those without a family history.
In addition, there are certain genetic conditions that are associated with an increased risk of GERD, such as hiatal hernia and scleroderma.
However, it is important to note that genetic factors are just one of many potential factors that can contribute to the development of GERD. Other factors, such as lifestyle choices (e.g., diet, smoking, alcohol consumption), obesity, and certain medical conditions (e.g., pregnancy, diabetes) can also increase the risk of GERD.
Is there a link between diabetes and gastroesophageal reflux disease (GERD)?
Yes, there is a link between diabetes and gastroesophageal reflux disease (GERD). Studies have found that individuals with diabetes are more likely to experience GERD than those without diabetes. The reasons for this are not completely understood, but it is thought that several factors may contribute to the association.
One possible explanation is that high blood sugar levels can affect the function of the lower esophageal sphincter (LES), which is a muscle that normally prevents stomach acid from flowing back up into the esophagus. When the LES doesn’t function properly, stomach acid can reflux into the esophagus, causing GERD symptoms.
Additionally, individuals with diabetes may also have slower emptying of the stomach, which can lead to increased pressure in the stomach and reflux of stomach acid into the esophagus. It is also worth noting that some medications commonly used to treat diabetes, such as metformin and insulin, may also contribute to GERD symptoms in some individuals.
Is gastroesophageal reflux disease (GERD) curable?
Gastroesophageal reflux disease (GERD) is not considered curable, but it can be effectively managed with proper treatment and lifestyle modifications.
The goal of treatment for GERD is to reduce the frequency and severity of symptoms and to prevent complications. Treatment options may include:
- Lifestyle modifications: Making changes to your diet and lifestyle can help to reduce symptoms of GERD. This may include avoiding certain trigger foods, losing weight, avoiding tight-fitting clothing, and elevating the head of your bed.
- Medications: Several medications are available to treat GERD, including antacids, H2 blockers, and proton pump inhibitors (PPIs). These medications work by reducing the amount of acid in the stomach, which can help to reduce symptoms of GERD.
- Surgery: In some cases, surgery may be recommended to treat GERD. This may involve a procedure to strengthen the lower esophageal sphincter (LES) or to create a barrier to prevent stomach acid from refluxing into the esophagus.
While GERD is not curable, with proper treatment and lifestyle modifications, most people with the condition are able to manage their symptoms effectively and prevent complications.
What is considered a refractory gastroesophageal reflux disease (GERD)?
Refractory gastroesophageal reflux disease (GERD) refers to GERD that does not respond to standard medical or surgical treatments, or that recurs despite treatment. The definition of refractory GERD can vary depending on the study or expert opinion, but generally, it is defined as GERD that persists despite a trial of at least 8-12 weeks of proton pump inhibitor (PPI) therapy at the maximum dose or twice-daily dosing. Refractory GERD may also be defined as GERD that persists despite other interventions, such as lifestyle modifications or surgery.
Individuals with refractory GERD may continue to experience symptoms such as heartburn, regurgitation, and chest pain despite treatment. Refractory GERD can be challenging to manage and may require further testing to identify the underlying cause of symptoms.
Treatment options for refractory GERD may include switching to a different type of acid-suppressing medication, such as a histamine-2 receptor antagonist (H2RA), or a combination of medications. In some cases, surgical interventions may be considered, such as fundoplication or the LINX device.
When is Nissen fundoplication indicated in gastroesophageal reflux disease (GERD)?
Nissen fundoplication is a surgical procedure that is sometimes recommended for the treatment of gastroesophageal reflux disease (GERD) in certain situations.
Nissen fundoplication may be indicated for individuals with severe GERD who:
- Do not respond to medication: If an individual’s GERD symptoms persist despite treatment with medications such as proton pump inhibitors (PPIs), surgery may be considered.
- Have complications of GERD: Nissen fundoplication may be recommended for individuals who have developed complications of GERD, such as respiratory symptoms.
- Cannot tolerate medication: In some cases, individuals may not be able to tolerate long-term use of medication due to side effects or other medical conditions.
Nissen fundoplication involves wrapping the upper part of the stomach around the lower esophageal sphincter (LES) to strengthen the barrier between the stomach and esophagus and prevent reflux. The procedure is usually done laparoscopically, which is a minimally invasive approach that involves small incisions and faster recovery time.
Nissen fundoplication is a major surgical procedure with potential risks and complications, and should only be considered after careful evaluation and discussion with a gastroenterologist.
How can I contact gastroenterologist Dr. Zavos for an appointment?
Dr. Chris Zavos is a board-certified gastroenterologist and hepatologist, located in Thessaloniki Greece, and specifically in Kalamaria suburb, about 7 kilometres (4 miles) southeast of downtown Thessaloniki. His private office is at: Fanariou 8 street (near Aigaiou and Adrianoupoleos avenues), Kalamaria (Thessaloniki), Greece.
Thessaloniki International Airport is only 10 km away from his private office in Kalamaria and can be reached by taxi within 13 minutes from the airport.
Dr. Chris Zavos performs endoscopies at Bioclinic private hospital in downtown Thessaloniki (Mitropoleos 86 street).
You can contact Dr. Zavos at phone numbers: (+30)-6976596988 and (+30)-2311283833, or you can email him at czavos@ymail.com. Dr. Zavos responds to Greek and English languages.
References
- Kountouras J, Zavos C, et al. Helicobacter pylori and gastro-oesophageal reflux disease. Lancet 2006 Sep 16-22;368(9540):986.
- Kountouras J, Zavos C, et al. Efficacy of trimebutine therapy in patients with gastroesophageal reflux disease and irritable bowel syndrome. Hepatogastroenterology 2002 Jan-Feb;49(43):193-7.
- Kountouras J, Zavos C, et al. H pylori infection and reflux oesophagitis. Gut 2004 Jun;53(6):912.
- Kountouras J, Zavos C, et al. Induction of interleukin-8 expression by Helicobacter pylori infection in patients with endoscopy-negative gastroesophageal reflux disease. Am J Gastroenterol 2004 Dec;99(12):2500-1.
- Kountouras J, Zavos C, et al. Eradication of Helicobacter pylori might halt the progress to oesophageal adenocarcinoma in patients with gastro-oesophageal reflux disease and Barrett’s oesophagus. Med Hypotheses 2007 May;68(5):1174-5.
- Kountouras J, Zavos C, et al. The role of gastric Helicobacter pylori infection in laryngopharyngeal reflux disease. Otolaryngol Head Neck Surg 2007 Feb;136(2):334.
- Kountouras J, Zavos C, et al. Helicobacter pylori infection might contribute to esophageal adenocarcinoma progress in subpopulations with gastroesophageal reflux disease and Barrett’s esophagus. Helicobacter 2012 Oct;17(5):402-3.
- Kountouras J, Zavos C, et al. Is Helicobacter pylori the usual suspect behind gastroesophageal reflux disease and dacryostenosis?. Med Hypotheses 2013 Jul;81(1):147.
- Richter JE, Rubenstein JH. Presentation and epidemiology of gastroesophageal reflux disease. Gastroenterology 2018;154:267-76.
- Katz PO, Dunbar KB, Schnoll-Sussman FH, Greer KB, Yadlapati R, Spechler SJ. ACG Clinical Guideline for the Diagnosis and Management of Gastroesophageal Reflux Disease. Am J Gastroenterol 2022;117:27-56.
- Fass R. Gastroesophageal Reflux Disease. N Engl J Med 2022;387:1207-1216.
