The role of upper gastrointestinal endoscopy (or gastroscopy or esophagogastroduodenoscopy) in gastroesophageal reflux disease diagnosis
Upper endoscopy is a pivotal tool for diagnosing gastroesophageal reflux disease (GERD), especially when patients exhibit concerning symptoms. Its primary role is to evaluate the condition of the esophageal mucosa. Here’s a detailed look into how upper endoscopy aids in the diagnosis of GERD, the significance of the Los Angeles (LA) classification, and the considerations regarding the use of proton pump inhibitors (PPIs) before endoscopy.
When to perform upper GI endoscopy (EGD)
- Immediate Need: For GERD patients displaying alarm symptoms like dysphagia (difficulty swallowing), significant weight loss, bleeding, frequent vomiting, and/or anemia, an upper endoscopy should be conducted promptly.
- Diagnostic Clarity: The procedure is crucial for identifying specific conditions such as erosive esophagitis (EE) and Barrett’s esophagus, which are indicative of GERD.
The LA Classification System
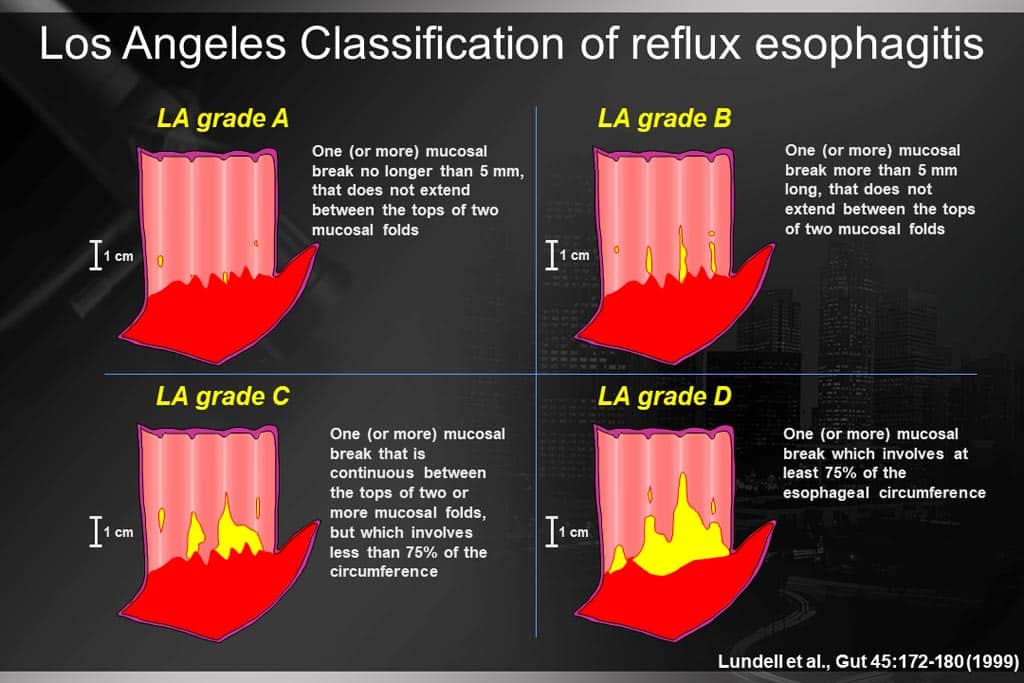
- Widely Adopted: The Los Angeles (LA) classification of EE is a validated and extensively used scoring system to assess the severity of esophageal erosions.
- Grading Severity:
- LA grade A EE is often indistinguishable from normal, thus not alone conclusive for GERD.
- LA grade B EE, alongside typical GERD symptoms and a positive response to PPI treatment, may diagnose GERD.
- LA grades C and D EE are more definitive, with grade D indicating severe GERD, especially in outpatient scenarios.
Barrett’s esophagus and GERD diagnosis
- A Barrett’s esophagus segment exceeding 3 cm, confirmed through biopsy, is diagnostic of GERD without the need for additional pH testing.
Considerations for PPI use before the upper GI endoscopy
- Common Findings: Normal mucosa is most often observed in patients undergoing endoscopy for GERD symptoms.
- Impact of PPIs: Given their effectiveness in healing EE, PPIs can mask underlying erosive disease, making it challenging to diagnose during endoscopy.
- Diagnostic Strategy:
- To improve the diagnostic accuracy for GERD and assess for EE, it’s advisable to halt PPI treatment for 2 to 4 weeks prior to endoscopy.
- This pause not only aids in diagnosing GERD but also in identifying eosinophilic esophagitis (EoE), which requires esophageal biopsies for confirmation.
Practical advice for patients
- PPI Discontinuation: Patients are encouraged to stop PPI therapy for 2 to 4 weeks before undergoing diagnostic endoscopy to maximize the chance of accurate diagnosis. Antacids or Chios mastic (Mastiha var. Chis caps.) can be used for symptom management during this period.
- Evaluating Treatment Efficacy: For those with LA grade C and D EE, post-PPI treatment endoscopy is recommended to confirm healing and check for Barrett’s esophagus, particularly challenging to detect amidst severe EE.
Conclusion
Upper endoscopy remains a cornerstone in diagnosing GERD, particularly for patients with alarming symptoms and when evaluating the efficacy of PPI therapy. The LA classification aids in assessing the severity of erosive esophagitis, while a temporary cessation of PPIs before the procedure enhances the likelihood of a precise diagnosis. Through these meticulous approaches, healthcare providers can ensure a comprehensive evaluation of GERD and related conditions.
