Is stool consistency an indicator of someone’s digestive health?
The consistency of your stool can provide important information about your digestive health. While the appearance and color of your poop can also be indicators of digestive issues, the consistency of your stool is often a more reliable and consistent measure of your digestive health. In this article, we’ll take a closer look at the different types of stool consistency, what they mean, and when you should be concerned.
What is the Bristol Stool Chart?
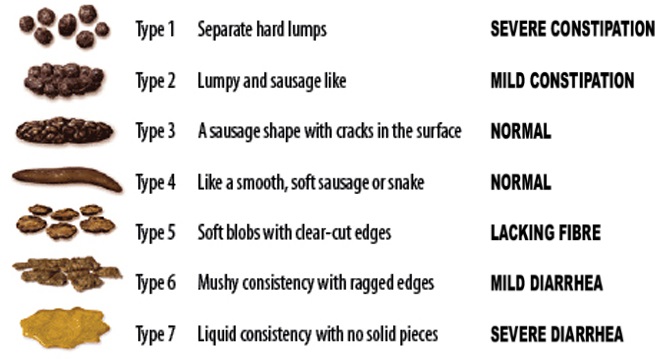
The Bristol Stool Chart is a medical tool used to classify the different types of stool based on their consistency and shape. It was first developed at the Bristol Royal Infirmary in the United Kingdom in 1997 and has since become a widely recognized tool for evaluating digestive health.
The chart consists of 7 types of stool, each with a corresponding image and description. These types range from hard, lumpy stool (Type 1) to entirely liquid stool (Type 7), with various textures and consistencies in between.
The purpose of the Bristol Stool Chart is to provide a standardized way of assessing bowel movements and to help healthcare providers identify potential digestive issues. By using the chart to describe their bowel movements, patients can help healthcare providers diagnose and treat issues like constipation, diarrhea, and other digestive problems.
The Bristol Stool Chart is a useful tool because it provides a clear visual representation of the different types of stool and their associated health implications. It also helps to reduce any discomfort or embarrassment patients may feel when discussing their bowel movements with their gastroenterologist, as it provides a more objective and clinical way of describing their symptoms.
Overall, the Bristol Stool Chart is a simple and effective tool that can be used by patients and gastroenterologists alike to evaluate and maintain optimal digestive health.
Type 1: Hard lumps
If your stool is hard and comes out in small, lumpy pieces, it may be a sign of constipation. This type of stool can be difficult to pass and may require straining, which can lead to hemorrhoids or anal fissures over time.
What to do: To prevent constipation, make sure you are drinking enough water and eating a fiber-rich diet. If constipation persists, talk to your gastroenterologist about over-the-counter laxatives or stool softeners.
Type 2: Sausage-shaped but lumpy
This type of stool is similar to Type 1 but has a more sausage-like appearance. It may also be difficult to pass and may require straining.
What to do: Same as for Type 1.
Type 3: Sausage-shaped with cracks
This type of stool is easier to pass than Types 1 and 2 but still has some degree of constipation. It appears sausage-like but has visible cracks on the surface.
What to do: Increase fiber intake and water consumption. Over-the-counter remedies like stool softeners and laxatives may help.
Type 4: Sausage or snake-like, smooth and soft
This is the ideal stool consistency. It’s easy to pass and indicates good digestive health. It should be similar in shape and texture to a sausage or snake and should come out smoothly.
What to do: Keep up the good work!
Type 5: Soft blobs with clear-cut edges
This type of stool is similar in consistency to Type 4 but is not as well-formed. It may have a softer texture and may come out in smaller pieces.
What to do: Make sure you are getting enough fiber and water. If this type of stool persists, talk to your gastroenterologist.
Type 6: Mushy consistency
This type of stool is softer and more liquid than Types 4 and 5. It may be easier to pass but may indicate mild diarrhea.
What to do: Monitor your symptoms and make sure you are staying hydrated. If diarrhea persists, talk to your gastroenterologist.
Type 7: Watery consistency
This type of stool is entirely liquid and is a sign of severe diarrhea. It may be accompanied by other symptoms like abdominal pain or cramping.
What to do: Stay hydrated and monitor your symptoms closely. If diarrhea persists for more than a few days or is accompanied by other concerning symptoms, talk to your gastroenterologist.
By paying attention to the consistency of your stool, you can gain important insights into your digestive health. While occasional changes in stool consistency are normal, persistent changes or concerning symptoms should be evaluated by a gastroenterologist. By maintaining a healthy diet, staying hydrated, and seeking medical attention when necessary, you can help promote optimal digestive health and overall well-being.
Big poop: Is it normal and healthy?
While the size of your poop can vary depending on your individual bowel habits and diet, passing a big poop from time to time is generally considered normal and healthy.
In fact, the size and shape of your poop can provide insights into your digestive health. Ideally, your poop should be long and smooth, similar to a sausage, and should be easy to pass without straining.
However, if you frequently experience difficulty passing large or hard stools, it may be a sign of constipation, which can be caused by a variety of factors, including dehydration, a lack of fiber in your diet, or certain medications. If you are experiencing persistent constipation or other digestive symptoms, it is important to speak with your gastroenterologist to determine the underlying cause and appropriate treatment.
What affects stool consistency?
Several factors can affect stool consistency, including:
- Diet: The types of food you eat can significantly impact the consistency of your stool. For example, a high-fiber diet can produce soft, bulky stools, while a low-fiber diet can result in hard, lumpy stools.
- Hydration: Dehydration can lead to hard, dry stools, while staying adequately hydrated can help keep stools soft and easy to pass.
- Medications: Some medications, such as opioids and certain antibiotics, can cause constipation and result in hard, lumpy stools.
- Digestive disorders: Certain digestive disorders, such as irritable bowel syndrome (IBS), inflammatory bowel disease (IBD), and celiac disease, can cause changes in stool consistency.
- Exercise: Regular exercise can help promote healthy digestion and regular bowel movements.
- Stress: High levels of stress can affect bowel movements and lead to changes in stool consistency.
- Medical conditions: Certain medical conditions, such as thyroid disorders and diabetes, can impact stool consistency.
It is essential to pay attention to changes in stool consistency, as they can be an indicator of digestive problems or other underlying health issues. If you notice significant or persistent changes in your stool consistency, it is a good idea to talk to your gastroenterologist to determine the cause and appropriate treatment.
What stool consistency should prompt me to seek help from my gastroenterologist?
If you experience any persistent changes in your stool consistency, it is a good idea to seek help from your gastroenterologist. Some changes in stool consistency that may indicate a problem include:
- Hard, lumpy stools that are difficult to pass or require straining
- Loose, watery stools that persist for more than a day or two
- Stools that are black or tarry in appearance
- Stools that are consistently pale or clay-colored
- Stools that contain blood or mucus
- Stools that have a foul or unusual odor
These changes in stool consistency could be a sign of an underlying digestive disorder, infection, or other health problem that requires medical attention. It is always better to err on the side of caution and seek medical advice if you are concerned about changes in your stool consistency or any other digestive symptoms. Your gastroenterologist can help diagnose the underlying cause of your symptoms and recommend appropriate treatment options.
You can also have a look at another article of peptiko.gr on the Poop Color Guide here.
You can also have a look at another article of peptiko.gr on the Stool Odor Guide here.
How can I contact gastroenterologist Dr. Zavos for an appointment?
Dr. Chris Zavos is a board-certified gastroenterologist and hepatologist, located in Thessaloniki Greece, and specifically in Kalamaria suburb, about 7 kilometres (4 miles) southeast of downtown Thessaloniki. His private office is at: Fanariou 8 street (near Aigaiou and Adrianoupoleos avenues), Kalamaria (Thessaloniki), Greece.
Thessaloniki International Airport is only 10 km away from his private office in Kalamaria and can be reached by taxi within 13 minutes from the airport.
Dr. Chris Zavos performs endoscopies at Bioclinic private hospital in downtown Thessaloniki (Mitropoleos 86 street).
You can contact Dr. Zavos at phone numbers: (+30)-6976596988 and (+30)-2311283833, or you can email him at czavos@ymail.com. Dr. Zavos responds to Greek and English languages.
