Helicobacter pylori and osteoporosis
Please click on the above YouTube video to watch the presentation of Dr. Christos Zavos on Helicobacter pylori and osteoporosis, to be presented at the Online Conference entitled: “OSTEOPOROSIS – ACTUAL MULTIDISCIPLINARY PROBLEM”, organized by: National Academy of Medical Sciences of Ukraine; Ministry of Health of Ukraine; D. F. Chebotarev Institute of Gerontology of the National Academy of Medical Sciences of Ukraine; and Ukrainian Association of Osteoporosis, Ukraine 17-18 November 2022
Introduction
Helicobacter pylori, a Gram-negative and spiral shaped bacterium dwelling on the gastric epithelium, has an influence on approximately 50% of the global population, especially those living in developing countries.
Osteoporosis is one of the most common metabolic bone diseases, characterized by decreased bone mineral density (BMD), increased bone fragility and then increased susceptibility to fracture, especially in spine and hip. Osteoporosis has become a major health concern for both individuals and societies. Osteoporosis has huge adverse impacts on life quality and is associated with increased morbidity rates.
Helicobacter pylori and osteoporosis: Similarities
There are similarities between these 2 clinical entities: Helicobacter pylori infection and osteoporosis:
- They both affect older ages
- They are both common multifactorial and heterogenic disorders of increasing incidence
- They both constitute major challenges for public health systems globally due to huge clinical and economic burdens
Helicobacter pylori prevalence
The prevalence of Helicobacter pylori infection is approximately 30% in developed countries, 80% in developing countries and up to 90% in patients with dyspepsia. In North Europe and North America, about one-third of adults are infected, and in South and East Europe, South America and Asia, the prevalence of Helicobacter pylori is often higher than 50%. Moreover, infected subjects born abroad (first-generation immigrants) had a higher risk of Helicobacter pylori infection than second-generation immigrants in Europe.
Osteoporosis prevalence
In Europe, about half of women and one-fifth of men aged over 50 years develop pathological fractures in hip, spine, forearm or humerus due to osteoporosis during their remaining lifetime. The same situation happens in other countries or districts, such as Japan and Taiwan.
In the Global map of health burden of low bone mineral density (LBMD)-related fractures in 2019 study, data from 204 countries and territories were analyzed. The five countries with the highest disability-adjusted life years number in fractures due to LBMD in 2019 were India; China; United States of America; Japan; and Germany. The countries with the highest number of deaths due to LBMD-related fractures in 2019, were India, China, United States of America, France, and Germany. As we can see from the map, this is the opposite compared with Helicobacter pylori prevalence which is higher in the developing countries, as mentioned earlier.
Helicobacter pylori and extraintestinal disorders associated with osteoporosis
Helicobacter pylori infection has been associated with numerous extraintestinal disorders, many of which have the potential to influence bone and muscle status, such as:
- autoimmune thyroid diseases
- diabetes mellitus
- dyslipidemia
- obesity
- osteoporosis
- primary hyperparathyroidism
The PhD thesis of Dr. Christos Zavos was on the relationship between Helicobacter pylori infection and glaucoma, another intriguing extraintestinal manifestation associated with Helicobacter pylori infection.
Osteoporosis has a multifactorial etiology
Osteoporosis is a major cause of bone fracture and subsequent morbidity and mortality in the elderly population. Several clinical and demographic parameters including:
- aging
- menopause
- parity
- inflammatory disease
- hormonal
- gastrointestinal
- renal
- metabolic disorders like vitamin D deficiency
- obesity
- weight loss
may affect bone mass and result in bone mineral density changes and osteoporosis.
Helicobacter pylori and osteoporosis association: Data from the most recent meta-analysis
In the most recent systematic review and meta-analysis to evaluate the association between Helicobacter pylori infection and osteoporosis, the overall odds ratio (OR) was obtained based on the 20 studies involving the Helicobacter pylori and osteoporosis (including osteopenia) (a total of 8788 patients and healthy controls). As the existence of obvious heterogeneity (χ2=69.60, I2=72.7%, P<0.01), random effect model was used and the pooled results of OR and its 95% condidence interval (CI) were 1.37 (1.11 to 1.69), indicating Helicobacter pylori infection was significantly associated with increased odds of osteoporosis/osteopenia.
Given that obvious heterogeneity existed, subgroup analyses were performed based on the potential confounding factors. All 20 studies were involved in these subgroup analyses. Here you can see both osteoporosis and osteopenia were significantly associated with Helicobacter pylori infection with OR (95% CI) of 1.61 (1.11 to 2.32) and 1.22 (1.07 to 1.39), respectively. Although the OR was a little higher in osteoporosis group, the meta regression analysis showed no significant difference between these two groups (t=1.18, P=0.26). The meta-analysis showed that the association between Helicobacter pylori infection and osteoporosis was significant in men and both sexes, but not in women.
When stratified by countries, the meta-analysis found significant associations between Helicobacter pylori infection and osteoporosis in China, Japan and Korea (three Asian countries), indicating many other factors associated with geography may affect the results.
The bone mineral density (BMD) (g/cm2) alterations between Helicobacter pylori-positive and Helicobacter pylori-negative participants were −0.01 (−0.45 to 0.42) for hip, −0.94 (−3.15 to 1.28) for lumber and −0.04 (-0.40 to 0.31) for femur using random effects model as obvious heterogeneity existed. No significant associations were observed.
Pathophysiological mechanisms by which Helicobacter pylori infection may contribute to osteoporosis
The pathophysiological mechanisms by which Helicobacter pylori infection may contribute to osteoporosis include the following:
- SYSTEMIC INFLAMMATION INDUCED BY H. PYLORI Helicobacter pylori induces the release of cytokines, such as TNF-α, IL-1 and IL-6, which may cause bone turnover indirectly
- LOW VITAMIN B12 ASSOCIATED WITH H. PYLORI If the serum vitamin B12 levels are decreased, the folate becomes trapped as methyltetrahydrofolate and interrupts folate-related DNA synthesis, an important factor for bone remodeling. Therefore, the decrease of vitamin B12 may lead to decreased BMD and osteoporosis.
- H. PYLORI MAY DECREASE CALCIUM ABSORPTION Helicobacter pylori causes gastric mucosal atrophy and decreases acid secretion. Thus, eradication of Helicobacter pylori may increase calcium absorption and stop the process of osteoporosis through decreasing the levels of inflammatory cytokines and improving gastric mucosal atrophy.
The Figure below, also shown in the video of Dr. Christos Zavos’s presentation, briefly outlines the mechanisms by which Helicobacter pylori infection and proton pump inhibitor (PPI) use may lead to an increased risk of osteoporosis and fracture.
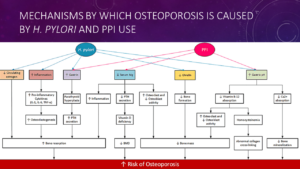
Helicobacter pylori infection as well as PPI use may lead to the release of proinflammatory cytokines and malabsorption of nutrients like Ca, Mg, and vitamin B12. It can also cause hormonal imbalance, including increased gastrin secretion and reduced ghrelin and circulating estrogen levels.
Regarding hormonal factors, chronic hypergastrinemia can occur as a result of hypochlorhydria/achlorhydria caused by Helicobacter pylori infection which can lead to parathyroid hyperplasia, resulting in increased parathormone (PTH) secretion and decreased BMD. PTH controls the level of calcium in the blood. Calcium is a mineral that keeps bones and teeth healthy and strong. It is also essential for the proper functioning of your nerves, muscles, and heart.
Furthermore, Helicobacter pylori infection can destroy gastric oxyntic glands that secrete ghrelin. Ghrelin, besides appetite stimulation, promotes osteoblast proliferation and differentiation. Lower ghrelin levels can decrease bone formation and increase the risk of bone fracture.
Finally, a decrease in total, free, and bioavailable estradiol levels was found in patients of both genders with Helicobacter pylori infection. The gastric parietal cells express aromatase enzyme and aid in the peripheral conversion of androgen to estrogen. The loss of gastric parietal cells due to Helicobacter pylori infection can thus lead to a decrease in the pool of estrogen, causing a potential link to bone fragility.
Limitations in the studies associating Helicobacter pylori infection to osteoporosis
The following limitations exist in the studies associating Helicobacter pylori infection to osteoporosis:
- SEROPOSITIVITY Helicobacter pylori infection is usually confirmed by serological testing, which cannot distinguish between current and past infection. Such a distinction is crucial to confirm an active systemic inflammation. In addition, seropositivity alone in elderly subjects without any dyspeptic symptoms cannot be considered as an active systemic inflammation.
- MULTIFACTORIAL ETIOLOGY Several factors may affect bone mass and make it impossible to determine the independent association between Helicobacter pylori infection and osteoporosis.
- CONFOUNDERS IN H. PYLORI INFECTION In patients with H. pylori infection many associated factors including dyspepsia, administration of PPIs, changes in diet, and disorder in calcium absorption may affect bone mass and confound the results.
- CONFOUNDERS IN OSTEOPOROSIS Patients’ older age, menopause, previous pregnancies and lack of physical activity due to knee osteoarthritis are the most common causes of BMD changes
- OTHER DISEASES INVOLVED IN OSTEOPOROSIS DEVELOPMENT Undiagnosed patients at earlier stage of inflammatory arthritis like rheumatoid arthritis are at greater risk of bone loss. Conditions such as chronic obstructive pulmonary disease and chronic renal disease are associated with inflammation and so are at greater risk of bone loss
- DEFINING OSTEOPOROSIS Diagnosis of osteoporosis based on the BMD T-score in older patients may underestimate the real prevalence of osteoporosis. Osteoarthritis is prevalent in older subjects and the presence of osteophytes results in falsely elevation of BMD and underestimation of osteoporosis particularly at the spine
- OSTEOARTHRITIS AS A CONFOUNDER Distribution and the severity of osteoarthritis may differ between the comparison groups
- DESIGN OF STUDIES Cross-sectional and case-control: Correlation does not indicate causation!
- DURATION OF ACTIVE H. PYLORI INFECTION The duration of active Helicobacter pylori infection and its contribution in the development of osteoporosis is difficult to be determined
- FEMALE SEX Sex of participants may affect the results: women and postmenopausal women are independent risk factors of osteoporosis. The relationship between osteoporosis and Helicobacter pylori infection was shown to be significant in men, but not in women
What should future studies focus on?
Future studies on Helicobacter pylori and bone mineral density require:
- A longitudinal assessment of the patients with active systemic inflammation confirmed by urea breath test or by gastric biopsy
- Nonetheless, treatment of patients with dyspepsia and active inflammation can affect the impact of Helicobacter pylori on BMD changes and confound the results
Concluding remarks
Taken together:
- Significantly increased odds of osteoporosis in patients with Helicobacter pylori infection
- The clinicians should pay more attentions to the patients infected with Helicobacter pylori by using DEXA scan, especially those patients with chronic gastritis
- The results should be cautiously interpreted considering the heterogeneity and the fact that all studies were non-randomized and retrospective
- Further studies are needed to explore the mechanisms and confounding factors between Helicobacter pylori and osteoporosis
References
- Hooi JKY, et al. Global Prevalence of Helicobacter pylori Infection: Systematic Review and Meta-Analysis. Gastroenterology 2017;153:420-429.
- Shen Y, et al. The Global Burden of Osteoporosis, Low Bone Mass, and Its Related Fracture in 204 Countries and Territories, 1990-2019. Front Endocrinol (Lausanne) 2022;13:882241.
- Wang T, et al. Relationship between Helicobacter pylori infection and osteoporosis: a systematic review and meta-analysis. BMJ Open 2019;9:e027356.
- Teresa Selvin S, et al. Establishing the Association Between Osteoporosis and Peptic Ulcer Disease: A Systematic Review. Cureus 2022;14:e27188.
- Pan BL, et al. Relationship between Helicobacter pylori infection and bone mineral density: a retrospective cross-sectional study. BMC Gastroenterol 2018;18:54.
- Heidari B. Helicobacter pylori infection and osteoporosis in elderly patients. Caspian J Intern Med 2015;6:48-50.
- Huang J, et al. The Association between Helicobacter pylori Seropositivity and Bone Mineral Density in Adults. Mediators Inflamm 2022;2022:2364666.
