What is nonalcoholic fatty liver disease (NAFLD)?
Nonalcoholic fatty liver disease (NAFLD) is a condition in which excess fat accumulates in the liver of people who drink little or no alcohol. It is a common condition that affects up to 25% of adults in the United States and is closely associated with obesity and type 2 diabetes.
Which are the 4 stages of nonalcoholic fatty liver disease (NAFLD)?
Non-alcoholic fatty liver disease (NAFLD) progresses through 4 main stages. Most people will only ever develop the first stage, which is a largely harmless build-up of fat in the liver cells known as simple fatty liver or steatosis. However, in a small number of cases, NAFLD can progress and eventually lead to liver damage if not detected and managed.
The more serious form of NAFLD is non-alcoholic steatohepatitis (NASH), where the liver becomes inflamed. Persistent inflammation can cause scar tissue to form around the liver and nearby blood vessels, leading to fibrosis. At this stage, the liver can still function normally.
However, if left untreated, NAFLD can progress to cirrhosis, the most severe stage, where the liver shrinks, becomes scarred and lumpy, and is permanently damaged. Cirrhosis can cause liver failure (where the liver stops working properly) and liver cancer (hepatocellular carcinoma). It can take years for fibrosis or cirrhosis to develop, so it is important to make lifestyle changes to prevent the condition from getting worse.
What is the exact cause of nonalcoholic fatty liver disease (NAFLD)?
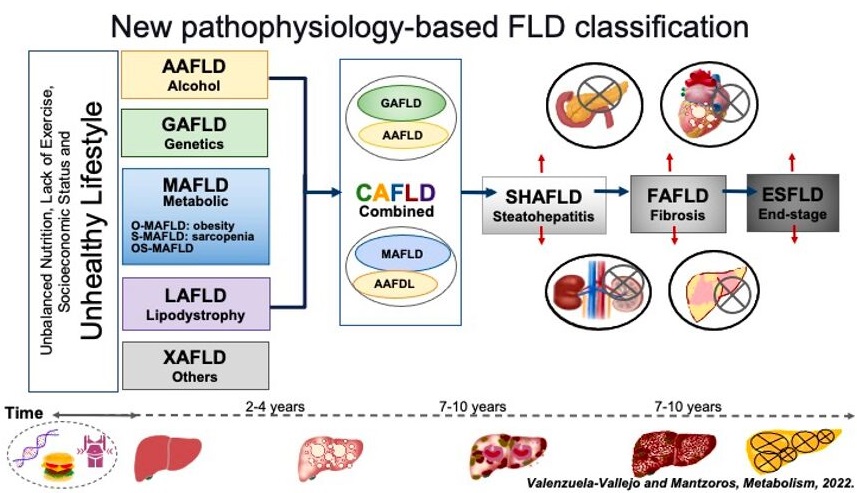
The exact cause of NAFLD is not well understood, but it is believed to be related to metabolic syndrome, insulin resistance, and oxidative stress. A new classification based on the pathophysiology of fatty liver disease (FLD) has recently been proposed, as shown in the Figure below.
Who is at risk to develop nonalcoholic fatty liver disease (NAFLD)?
Non-alcoholic fatty liver disease (NAFLD) is a condition that can affect anyone, but certain factors increase your risk. If you are obese or overweight, especially with excess fat around your waist (an “apple-like” body shape), have type 2 diabetes, insulin resistance, polycystic ovary syndrome, an underactive thyroid, high blood pressure, high cholesterol, metabolic syndrome (a combination of diabetes, high blood pressure, and obesity), over the age of 50 or smoke, you are at an increased risk of developing NAFLD.
However, NAFLD can also be diagnosed in individuals without any of these risk factors, including young children. It is important to note that unlike alcoholic liver disease (ALD), NAFLD is not caused by excessive alcohol consumption.
What are the main symptoms of nonalcoholic fatty liver disease (NAFLD)?
In the early stages of NAFLD, there are usually no symptoms, and individuals may not realize they have the condition until it is detected during tests performed for another reason. However, in some cases, people with NASH or fibrosis (more advanced stages of NAFLD) may experience dull or aching pain in the upper right abdomen (over the lower right side of the ribs), extreme tiredness, unexplained weight loss, and weakness. As cirrhosis (the most advanced stage) develops, more severe symptoms can occur, such as jaundice (yellowing of the skin and whites of the eyes), itchy skin, and swelling in the legs, ankles, feet, or abdomen (edema).
Is nonalcoholic fatty liver disease (NAFLD) diagnosed through specific tests?
To diagnose nonalcoholic fatty liver disease (NAFLD), doctors usually start with a liver function test to check for abnormal liver enzyme levels. However, NAFLD can be asymptomatic, so additional tests may be necessary to confirm the diagnosis.
An ultrasound scan of the abdomen may reveal a build-up of fat in the liver, and can be used to diagnose simple fatty liver (steatosis). If further evaluation is needed, a FibroScan or a specialized blood test may be ordered to determine the stage of the disease.
A biopsy may also be recommended to confirm the diagnosis and assess the degree of liver damage. During this procedure, a small sample of liver tissue is taken using a needle and sent to a laboratory for analysis. Other imaging tests, such as a CT scan or MRI, may also be used to assess liver health and diagnose any potential complications.
What 10 tips would Dr. Zavos, board-certified gastroenterologist in Thessaloniki Greece, recommend to the patients with nonalcoholic fatty liver disease (NAFLD)?
Many people with fatty liver disease reach out to me for advice on treatment. If you’re looking to modify or reverse the condition, here are ten helpful tips:
- Incorporate exercise into your routine. Studies have shown that aerobic exercise, resistance training, and high-intensity interval training all have benefits on fatty liver.
- Watch your calorie intake. Low calorie dietary interventions have been found to be the most effective. Aim for a daily intake of 1000 to 1500 calories with a deficit of 500-750 calories. Additionally, the Mediterranean diet without alcohol has shown to be helpful.
- Get enough sleep. Poor sleep, inadequate sleep (less than 6 hours), non-restorative sleep, and daytime napping for more than 60 minutes are all associated with new onset or worsening of fatty liver. Ensure that you prioritize getting enough quality sleep.
- Consider drinking coffee. While tea lovers might not appreciate it, studies have shown that coffee intake can reduce fatty liver disease. Ideally, consume black coffee without sugar or milk, at least three cups a day, and avoid drinking it late in the evening or at night. This dose of coffee is safe and may even lower blood pressure.
- Limit or eliminate alcohol consumption. Alcohol use is a leading cause of fatty liver, so the safest level of alcohol consumption to prevent fatty liver is zero. Switch to non-alcoholic beverages with low calories instead. NAFLD may not be caused by alcohol, but drinking alcohol may deteriorate NAFLD.
- Avoid sugar-sweetened beverages and processed foods that contain fructose. These items can significantly increase liver fat and have been linked to fatty liver in both children and adults.
- Use artificial sweeteners with caution. Although artificial sweeteners are generally safer than natural sugars, studies have shown that they may increase liver fat in animal models due to their effects on gut bacteria. Stevia is considered the safest artificial sweetener. If you have diabetes or obesity, talk to your healthcare provider before using artificial sweeteners.
- Be cautious with drug therapy. There are currently no FDA-approved drugs for treating fatty liver disease, but vitamin E and pioglitazone are recommended by some experts. No other drugs have been shown to be effective. Drug therapy should only be initiated in individuals with confirmed nonalcoholic steatohepatitis (NASH) ideally through biopsy or noninvasive tests like Fibroscan/Shearwave. It is important not to initiate treatment based solely on an ultrasound scan identifying fatty liver. Drug therapy is typically not used for a lifetime but rather until other associated risk factors are under control.
- Take a rational approach to treating fatty liver. Fatty liver disease is actually a misnomer; it is not a disease but rather an association with underlying causes such as alcohol use, diabetes, obesity, hypothyroidism, sleep disorders, and a sedentary lifestyle. Therefore, treatments should focus on controlling these underlying causes instead of the liver itself. For more information on management and updates, refer to the 2022 American Association of Clinical Endocrinology (AACE) guidelines for nonalcoholic fatty liver disease.
- Be aware of what does not work. Ursodeoxycholic acid, milk thistle, green tea, omega-3 supplements, detox products, yoga (because it is not aerobic), fruitarian diets, crash diets, turmeric/cinnamon supplements, shifting to honey or coconut sugars, herbal formulations, multiherbal products, and any product labeled as a “liver detox” or “reverse fatty liver” are not effective treatments for fatty liver disease. For example, omega-3 fatty acids have been shown to reduce the amount of fat stored in liver cells, which can help improve liver health in individuals with non-alcoholic fatty liver disease (NAFLD). However, while omega-3 supplements may have a modest effect on reducing liver cell inflammation, they do not have any significant impact on liver fibrosis, which is a more serious stage of the disease. Therefore, omega-3 supplements are not typically recommended as a specific treatment for non-alcoholic steatohepatitis (NASH) or advanced stages of NAFLD.
How can I contact gastroenterologist Dr. Zavos for an appointment?
Dr. Chris Zavos is a board-certified gastroenterologist and hepatologist, located in Thessaloniki Greece, and specifically in Kalamaria suburb, about 7 kilometres (4 miles) southeast of downtown Thessaloniki. His private office is at: Fanariou 8 street (near Aigaiou and Adrianoupoleos avenues), Kalamaria (Thessaloniki), Greece.
Thessaloniki International Airport is only 10 km away from his private office in Kalamaria and can be reached by taxi within 13 minutes from the airport.
Dr. Chris Zavos performs endoscopies at Bioclinic private hospital in downtown Thessaloniki (Mitropoleos 86 street).
You can contact Dr. Zavos at phone numbers: (+30)-6976596988 and (+30)-2311283833, or you can email him at czavos@ymail.com. Dr. Zavos responds to Greek and English languages.
References
- Kountouras J, Zavos C, et al. Helicobacter pylori might contribute to nonalcoholic fatty liver disease–related cardiovascular events by releasing pro-thrombotic and pro-inflammatory factors. Hepatology 2014; (in press)
- Polyzos SA, Zavos C, et al. Nonalcoholic fatty liver disease: the pathogenetic roles of insulin resistance and adipocytokines. Curr Mol Med 2009 Apr;9(3):299-314.
- Polyzos SA, Zavos C, et al. Nonlinear distribution of adiponectin in patients with nonalcoholic fatty liver disease limits its use in linear regression analysis. J Clin Gastroenterol 2010 Mar;44(3):229-30.
- Polyzos SA, Zavos C, et al. Adipocytokines in insulin resistance and non-alcoholic fatty liver disease: the two sides of the same coin. Med Hypotheses 2010 Jun;74(6):1089-90.
- Polyzos SA, Zavos C, et al. The role of adiponectin in the pathogenesis and treatment of non-alcoholic fatty liver disease. Diabetes Obes Metab 2010 May;12(5):365-83.
- Polyzos SA, Zavos C, et al. The potential adverse role of leptin resistance in nonalcoholic fatty liver disease: a hypothesis based on critical review of literature. J Clin Gastroenterol 2011 Jan;45(1):50-4.
- Polyzos SA, Zavos C, et al. Adiponectin in non-alcoholic fatty liver disease treatment: therapeutic perspectives and unresolved dilemmas. Int J Clin Pract 2011 Mar;65(3):373-4.
- Polyzos SA, Zavos C, et al. Effect of spironolactone and vitamin E on serum metabolic parameters and insulin resistance in patients with nonalcoholic fatty liver disease. J Renin Angiotensin Aldosterone Syst 2011 Dec;12(4):498-503.
- Polyzos SA, Zavos C, et al. The emerging role of endocrine disruptors in the pathogenesis of insulin resistance: a hypothesis implicating nonalcoholic fatty liver disease. Curr Mol Med 2012 Jan;12(1):68-82.
- Polyzos SA, Zavos C, et al. Serum vitamin B12 and folate levels in patients with non-alcoholic fatty liver disease. Int J Food Sci Nutr 2012 Sep;63(6):659-66.
- Polyzos SA, Zavos C, et al. Nonalcoholic fatty liver disease: multimodal treatment options for a pathogenetically multiple-hit disease. J Clin Gastroenterol 2012 Apr;46(4):272-84.
- Polyzos SA, Zavos C, et al. Helicobacter pylori infection in patients with nonalcoholic fatty liver disease. Metabolism 2013 Jan;62(1):121-6.
- Polyzos SA, Zavos C, et al. Serum ferritin in patients with nonalcoholic fatty liver disease: evaluation of ferritin to adiponectin ratio and ferritin by homeostatic model of assessment insulin resistance product as non-invasive markers. Immunogastroenterology 2012 Oct;1(2):119-26.
- Polyzos SA, Zavos C, et al. Adipocytokines and cytokeratin-18 in patients with nonalcoholic fatty liver disease: introduction of CHA index. Ann Hepatol 2013 Sep-Oct;12(5):749-57.
- Polyzos SA, Zavos C, et al. Sex steroids and sex hormone-binding globulin in postmenopausal women with nonalcoholic fatty liver disease. Hormones (Athens) 2013 Jul-Sep;12(3):405-16.
- Polyzos SA, Zavos C, et al. Helicobacter pylori infection, insulin resistance and nonalcoholic fatty liver disease. Med Hypotheses 2014 Jun;82(6):795.
- Polyzos SA, Zavos C, et al. Nonalcoholic fatty liver disease and adipokines. In: Preedy VR, Hunter RJ (eds). Modern Insights into Disease from Molecules to Man: Adipokines. 1st Edn, Enfield NH, USA: Science Publishers, 2011.
- Simon TG, Henson J, Osganian S, et al. Daily aspirin use associated with reduced risk for fibrosis progression in patients with nonalcoholic fatty liver disease. Clin Gastroenterol Hepatol 2019;17:2776-2784.e4.
- Eslam M, Sanyal AJ, George J; International Consensus Panel. MAFLD: A Consensus-Driven Proposed Nomenclature for Metabolic Associated Fatty Liver Disease. Gastroenterology 2020;158:1999-2014.e1.
- Valenzuela-Vallejo L, Mantzoros CS. Time to transition from a negative nomenclature describing what NAFLD is not, to a novel, pathophysiology-based, umbrella classification of fatty liver disease (FLD). Metabolism 2022 Jul 1;134:155246.
- Riazi K, Azhari H, et al. The prevalence and incidence of NAFLD worldwide: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol 2022;7:P851-P861.
- Long MT, Noureddin M, Lim JK. AGA Clinical Practice Update: Diagnosis and Management of Nonalcoholic Fatty Liver Disease in Lean Individuals: Expert Review. Gastroenterology 2022 Jul 13:S0016-5085(22)00628-X.
- Cusi K, Isaacs S, Barb D, et al. American Association of Clinical Endocrinology Clinical Practice Guideline for the Diagnosis and Management of Nonalcoholic Fatty Liver Disease in Primary Care and Endocrinology Clinical Settings: Co-Sponsored by the American Association for the Study of Liver Diseases (AASLD). Endocr Pract 2022 May;28(5):528-562.
