Low FODMAP Diet: A Comprehensive Guide for Managing Digestive Disorders
The Low FODMAP diet is an evidence-based nutritional approach designed to alleviate symptoms associated with functional gastrointestinal disorders such as irritable bowel syndrome (IBS) and other similar conditions. Developed by researchers at Monash University in Australia, this diet targets the reduction of specific carbohydrates that are poorly absorbed by the gut and can cause significant discomfort. This article explores the fundamentals of the Low FODMAP diet, its benefits, and how it can be implemented effectively.
Understanding FODMAPs
FODMAPs are a group of fermentable carbohydrates and sugar alcohols, including fructose, lactose, fructans, galactans, and polyols. These substances are found in a wide range of foods, from dairy products and wheat to certain fruits and vegetables.
Here’s a breakdown of each type:
- Oligosaccharides: These include fructans and galacto-oligosaccharides (GOS). Common sources are wheat, rye, onions, garlic, and legumes/pulses.
- Disaccharides: The primary disaccharide in this group is lactose, found in dairy products like milk, soft cheeses, and yogurt.
- Monosaccharides: Fructose is a key monosaccharide, particularly when it is present in greater amounts than glucose in certain fruits and foods. Examples include apples, honey, and high-fructose corn syrup.
- Polyols: These are sugar alcohols like sorbitol and mannitol, which are found in some fruits and vegetables including mushrooms, stone fruits, and used as artificial sweeteners.
In sensitive individuals, FODMAPs are not well-absorbed in the small intestine and subsequently ferment in the large intestine, leading to the production of gas and attracting water, which can result in bloating, gas, abdominal pain, diarrhea, and constipation.
Principles of the Low FODMAP Diet
The diet is typically implemented in three phases:
- Elimination: High FODMAP foods are completely avoided for a period, usually 4-6 weeks, to allow for a clear assessment of whether symptoms improve when these foods are not consumed.
- Reintroduction: After the elimination phase, high FODMAP foods are gradually reintroduced into the diet one at a time. This process helps to identify specific foods that trigger symptoms.
- Personalization: Once the triggers are identified, they are limited or avoided according to individual tolerance, while other FODMAPs are reincorporated back into the diet.
Foods to Eat and Avoid
High FODMAP Foods to Limit or Avoid
High FODMAP foods can trigger digestive symptoms such as bloating, gas, and abdominal pain in sensitive individuals. Here is a more detailed list of common high FODMAP foods:
- Fruits: Apples, pears, mangoes, watermelon, cherries, and peaches.
- Vegetables: Onions, garlic, cauliflower, mushrooms, asparagus, and artichokes.
- Legumes and Pulses: Beans, lentils, chickpeas, and soybeans.
- Dairy Products: Milk (from cows, goats, and sheep), ice cream, and soft cheeses such as cottage cheese and ricotta.
- Wheat Products: Bread, pasta, cereals, and crackers made from wheat.
- Sweeteners: Honey, agave nectar, and products containing high fructose corn syrup, sorbitol, mannitol, and xylitol.
Low FODMAP Alternatives
Low FODMAP foods are generally easier for the gut to absorb and less likely to ferment in the large intestine. Incorporating these foods can help maintain a balanced diet while managing gastrointestinal symptoms:
- Fruits: Bananas, blueberries, strawberries, oranges, and grapes.
- Vegetables: Carrots, zucchini, spinach, tomatoes, bell peppers, and the green parts of spring onions and leeks.
- Dairy Alternatives: Lactose-free milk and yogurts, hard cheeses (such as cheddar, parmesan), and non-dairy alternatives like almond milk and coconut yogurt.
- Grains: Gluten-free bread and pasta, rice, oats, and quinoa.
- Protein: Eggs, firm tofu, and meats such as chicken, beef, and fish.
- Nuts and Seeds: Almonds (limit to 10 nuts per serving), macadamia nuts, peanuts, pumpkin seeds, and sesame seeds.
- Sweeteners: Maple syrup, glucose, and artificial sweeteners not derived from polyols (such as aspartame).
Benefits of the Low FODMAP Diet
The Low FODMAP diet, designed to reduce the intake of certain carbohydrates that can cause digestive distress, offers significant benefits for individuals suffering from gastrointestinal disorders such as irritable bowel syndrome (IBS). This dietary approach is scientifically backed and has been proven effective in managing symptoms in a substantial percentage of patients.
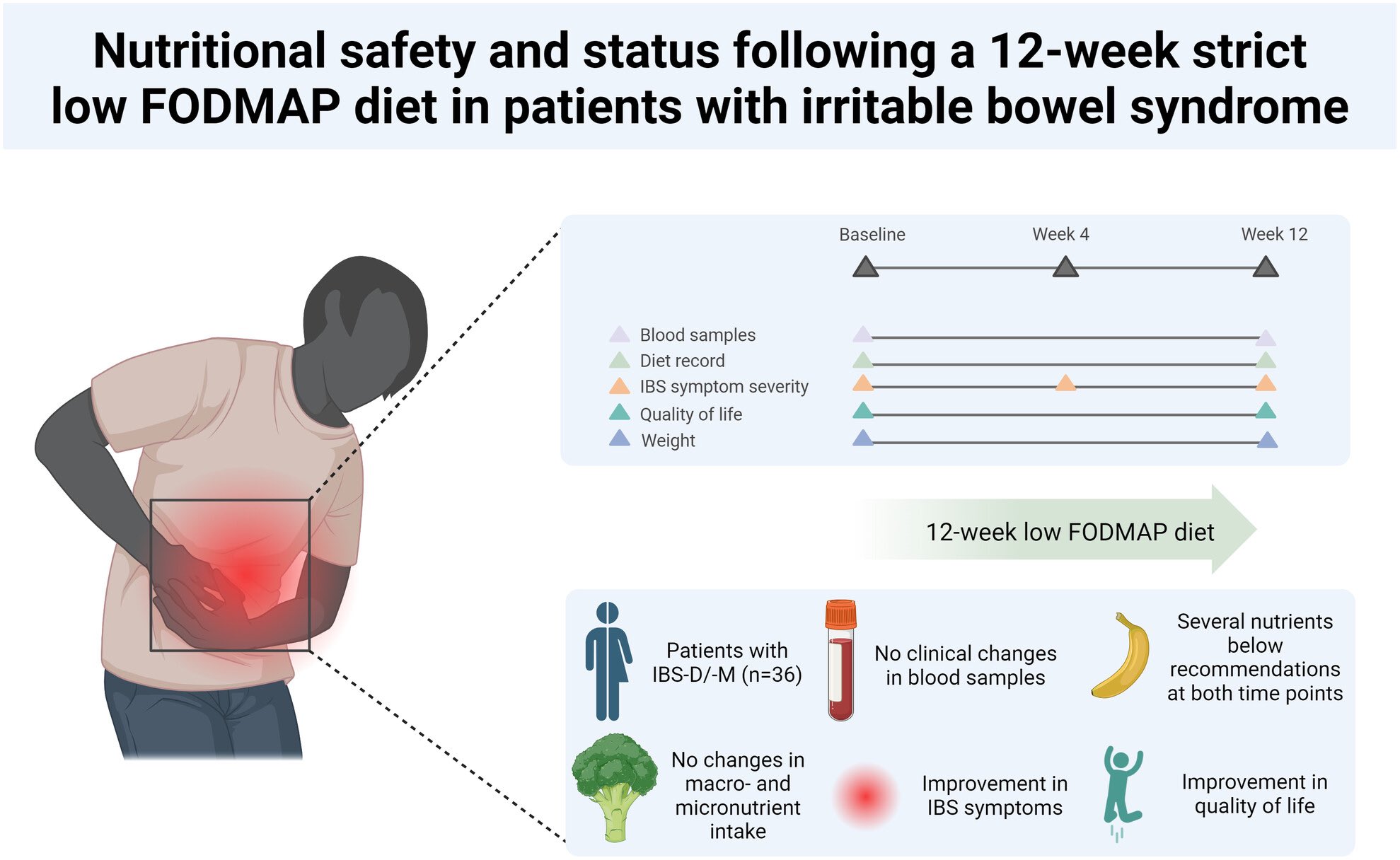
In a 12-week strict Low FODMAP Diet (LFD) study led by dietitians for patients with IBS-D and IBS-M, significant findings were observed concerning the dietary intake and quality of life (QoL) among participants. Despite the strict dietary guidance, there was no notable change in the intake of macro- and micronutrients from the start to the end of the study, nor were there any clinically meaningful differences in the various blood parameters measured. However, there was a slight decrease in the participants’ mean Body Mass Index (BMI) from 25.5 kg/m2 to 25.0 kg/m2. Notably, the Quality of Life scores significantly improved across nearly all assessed subdomains, with 80% of participants responding positively to the diet, underscoring the potential benefits of LFD in managing IBS symptoms and enhancing life quality.
The study further highlighted that many participants did not meet the recommended intake levels for several essential nutrients according to the Nordic Nutritional Recommendations, both at the beginning and end of the intervention. These deficiencies, which included nutrients like fiber, riboflavin, vitamin C, and iron, suggest that the baseline diet of the IBS cohort was of poor quality and potentially lacking in multiple areas. This underscores the critical role of dietitians in assessing and guiding patients on dietary modifications not only for symptom management but also to ensure overall nutritional adequacy. The strict LFD led to a significant reduction in fructan intake, which was linked to symptom improvement, reinforcing the importance of specialized dietary interventions in the management of IBS.
Here are the key benefits of following a Low FODMAP diet:
1. Reduction in Digestive Symptoms
The primary benefit of the Low FODMAP diet is the reduction of common and debilitating symptoms associated with digestive disorders, including:
- Bloating and Gas: By limiting foods that ferment in the large intestine, the diet can significantly reduce gas production and the associated bloating.
- Diarrhea and Constipation: The diet helps to normalize bowel movements by reducing the osmotic effects caused by poorly absorbed carbohydrates, which can alleviate both diarrhea and constipation.
- Abdominal Pain: Many patients report a significant reduction in the severity and frequency of abdominal pain and discomfort.
2. Improved Quality of Life
Digestive symptoms can severely affect one’s quality of life, impacting daily activities and mental health. Patients who adhere to a Low FODMAP diet often experience:
- Enhanced Emotional Wellbeing: Reduction in symptoms can lead to improvements in mood and decreased anxiety related to digestive issues.
- Greater Social Confidence: With fewer symptoms, individuals feel more confident in social situations without the fear of sudden digestive discomfort.
3. Enhanced Understanding of Personal Food Triggers
The structured reintroduction phase of the Low FODMAP diet enables individuals to identify specific foods that trigger their symptoms. This personalized knowledge allows for:
- Tailored Diets: Individuals can create a customized diet that avoids their specific triggers, while still enjoying a wide range of other foods.
- Control Over Symptoms: Understanding and controlling dietary triggers can provide a sense of empowerment and improved management over one’s health.
4. Potential Long-Term Intestinal Health Benefits
While the immediate goal of the Low FODMAP diet is symptom management, there may be potential long-term benefits for intestinal health, including:
- Reduced Inflammation: By avoiding trigger foods, individuals may experience reduced gut inflammation.
- Improved Gut Microbiota: Some studies suggest that long-term adjustments in diet can lead to a healthier balance of gut microbiota, although the specific impacts of the Low FODMAP diet on gut flora are still under investigation.
What is the FODMAP-light approach?
The FODMAP-light approach is an alternative to the traditional low-FODMAP diet, designed to provide symptom relief for individuals with IBS while minimizing dietary restrictions. This simplified method focuses on reducing only the most common and problematic high-FODMAP foods, such as onions, garlic, and certain legumes, rather than eliminating all high-FODMAP categories. By targeting key triggers, the FODMAP-light approach offers a more practical and less burdensome dietary plan that still delivers meaningful symptom improvement. Studies suggest that this method can be particularly effective for patients with mild-to-moderate IBS symptoms, enabling them to benefit from dietary intervention without the complexities of a full low-FODMAP regimen.
This approach is especially valuable for those who face challenges with the extensive planning and monitoring required by a traditional low-FODMAP diet. It allows for greater flexibility in food choices, making it easier to maintain social eating habits and cultural food preferences. The FODMAP-light strategy can also serve as a first-line dietary intervention for individuals hesitant to commit to more intensive dietary changes. By working with a dietitian or gastroenterologist, patients can identify which high-FODMAP foods are most problematic for them and focus on those specific eliminations. This targeted approach reduces dietary anxiety, enhances adherence, and offers a sustainable way to manage IBS symptoms while maintaining a balanced and enjoyable diet.
Conclusion
The Low FODMAP diet is a valuable intervention for managing symptoms of gastrointestinal disorders, but it can be complex and challenging to implement without expert guidance. Dr. Christos Zavos, a board-certified gastroenterologist and hepatologist in Thessaloniki, Greece, specializes in dietary management for gastrointestinal health. For professional advice on adopting the Low FODMAP diet or to discuss its appropriateness for your condition, potential patients are encouraged to reach out via the contact form on peptiko.gr, call at (+30)-6976596988 or (+30)-2311283833, or email czavos@ymail.com. A personalized approach ensures that patients receive the maximum benefits while minimizing any nutritional deficiencies or undue restrictions in their diet.
Reference
- Hillestad EMR, Steinsvik EK, Teige ES, et al. Nutritional safety and status following a 12-week strict low FODMAP diet in patients with irritable bowel syndrome. Neurogastroenterol Motil 2024 Apr 30:e14814.
