Hepatocellular Carcinoma (HCC) Treatment
Hepatocellular carcinoma (HCC) remains a challenging cancer to treat due to its complex pathophysiology and the varying underlying liver conditions of patients. Recent advancements and the consolidation of various treatment modalities provide a clearer roadmap for clinicians managing HCC. This article outlines the consolidated guidelines and recommendations for the treatment of HCC, emphasizing surgical interventions, liver transplantation, ablative therapies, intra-arterial treatments, and systemic therapies.
Surgical Resection
Surgical resection is often the preferred treatment for HCC in non-cirrhotic livers due to the less complicated liver status and the absence of cirrhosis-related complications. For HCC in cirrhotic livers, the decision to proceed with resection depends on multiple factors including liver function, the extent of portal hypertension, and the anticipated volume of the remaining liver post-surgery. Laparoscopic approaches are recommended where feasible, providing benefits such as reduced recovery time and fewer complications. Specific clinical scenarios, such as multifocal disease or tumors with vascular invasion, might also warrant consideration of resection, albeit with weaker recommendations due to varying degrees of evidence and efficacy.
Liver Transplantation
Liver transplantation (LT) offers a curative option for patients with decompensated cirrhosis or those who have HCC within specific tumor burden criteria. It is considered first-line treatment for such cases, with stringent selection criteria ensuring that only patients likely to benefit are chosen. For solitary small HCCs, LT might be considered if surgical resection or thermal ablation isn’t feasible. Neoadjuvant locoregional therapies are recommended while patients await transplantation to prevent disease progression and provide insights into tumor biology.
Ablative Therapy
For smaller tumors (<3 cm), thermal ablation—using techniques such as radiofrequency or microwave ablation—is preferred. This method is less invasive than surgical options and is especially useful for patients who are not suitable candidates for surgery. Percutaneous ethanol injection is an alternative for very small tumors (<2 cm) where thermal ablation isn’t feasible.
Intra-arterial Treatment
Transarterial embolization (TAE), conventional transarterial chemoembolization (cTACE), and drug-eluting bead TACE (DEB-TACE) are standard care for patients with intermediate-stage HCC. These methods are best suited for patients with limited tumor burden and preserved liver function. The choice between these techniques remains dependent on individual patient factors and institutional preferences, as evidence does not strongly favor one over the others.
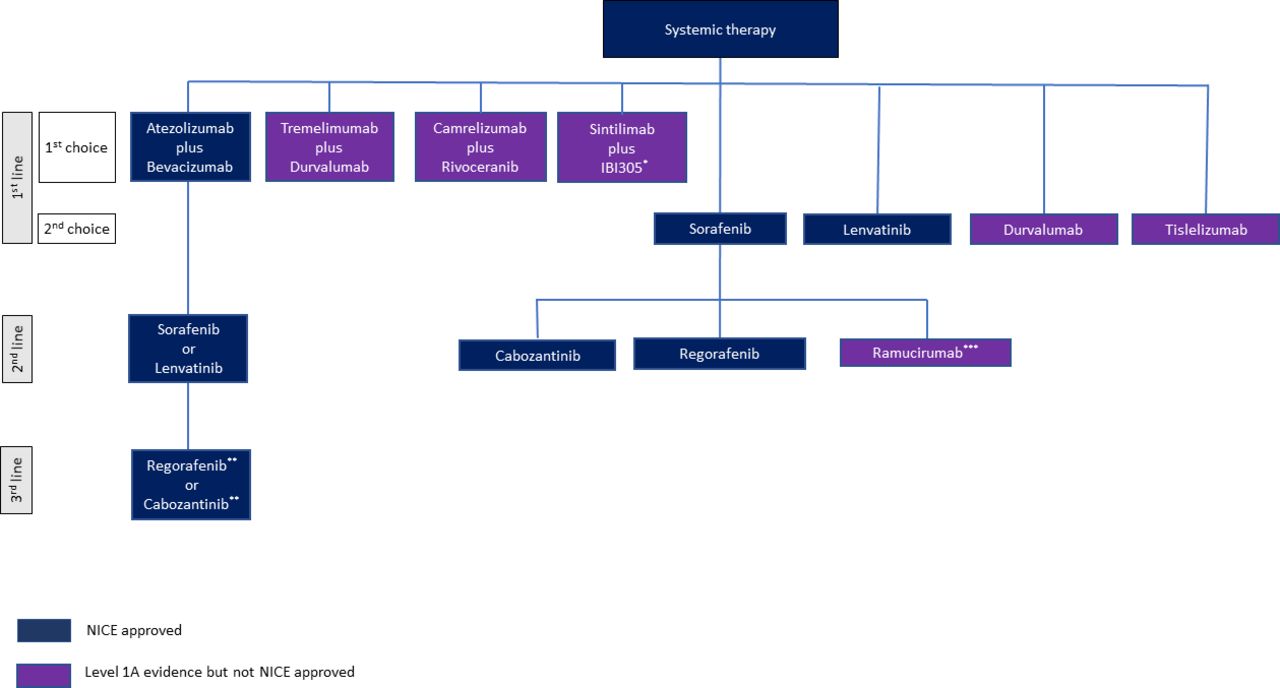
Systemic Therapy
Systemic therapy plays a pivotal role in the treatment of advanced hepatocellular carcinoma (HCC), particularly for patients with unresectable tumors, significant liver impairment, or metastatic disease. The landscape of systemic therapy for HCC has evolved dramatically over the past few years with the introduction of novel therapeutic agents and combinations that target different aspects of tumor growth and proliferation. Below, we explore the current options, their mechanisms, and their implications in clinical practice.
First-Line Systemic Therapy
- Atezolizumab and Bevacizumab Combination: This combination has emerged as the standard first-line treatment for advanced HCC. Atezolizumab, an immune checkpoint inhibitor that targets the PD-L1 pathway, enhances the immune response against cancer cells, while bevacizumab, an anti-angiogenic agent that inhibits VEGF, restricts tumor growth by reducing its blood supply. The synergy between these mechanisms has shown a significant improvement in overall survival and progression-free survival compared to previous standards such as sorafenib. Before initiating treatment, patients must be assessed for potential contraindications such as risk of gastrointestinal bleeding, particularly in those with known varices, necessitating recent endoscopic evaluation and management.
- Sorafenib and Lenvatinib: Both are tyrosine kinase inhibitors (TKIs) that block pathways involved in tumor cell proliferation and angiogenesis. Sorafenib has long been a cornerstone of HCC treatment, with lenvatinib emerging as a viable alternative due to its similar efficacy but different side effect profile, which may be preferable depending on the patient’s health status and existing comorbidities. The choice between these two agents often hinges on factors like tolerance and specific patient-related outcomes, such as response rate and progression-free survival.
Alternative First-Line Therapies
- Durvalumab and Tremelimumab: This combination represents a newer class of treatment involving dual immune checkpoint inhibition. Durvalumab targets PD-L1, and tremelimumab targets CTLA-4, another checkpoint protein on T cells. Early results suggest that this combination could be effective, with potentially lower risks of certain side effects compared to the atezolizumab-bevacizumab combination, although it is not yet widely approved.
- Sintilimab and IBI305; Camrelizumab and Rivoceranib: These combinations have shown promising results in the Asian population and are alternatives to sorafenib. Sintilimab and camrelizumab are PD-1 inhibitors, while IBI305 and rivoceranib act as anti-angiogenic agents. Their effectiveness compared to traditional therapies in non-Asian populations and broader international acceptance are areas of ongoing research.
Second-Line Systemic Therapy
- Tyrosine Kinase Inhibitors (TKIs) After Immunotherapy: For patients whose disease progresses after first-line treatment with atezolizumab and bevacizumab, second-line options include TKIs like regorafenib and cabozantinib. These drugs are approved for use following progression on sorafenib and have shown benefits in overall survival in this setting.
- Ramucirumab: This agent is a monoclonal antibody against VEGFR-2, effective as a second-line treatment particularly in patients with elevated alpha-fetoprotein (AFP) who have progressed on sorafenib. Its use might be expanded following future approvals based on ongoing clinical trial results.
When selecting systemic therapies, clinicians must consider several factors including the liver function, performance status of the patient, and specific molecular or biomarker profiles that may guide therapy selection. Despite the advances, there is a continuous need for the development of biomarkers that can predict response to these therapies and help tailor treatments more effectively.
Conclusion
The treatment of HCC requires a multidimensional approach tailored to the patient’s specific clinical profile and liver disease status. With ongoing research and the introduction of new therapeutic agents, the management of HCC continues to advance, offering hope for improved outcomes in this complex patient population. Clinicians must stay abreast of these developments and integrate multiple treatment modalities to optimize care for individuals affected by HCC.
Reference
- Suddle A, Reeves H, Hubner R, et al. British Society of Gastroenterology guidelines for the management of hepatocellular carcinoma in adults. Gut 2024 Apr 16:gutjnl-2023-331695.
