Hepatitis B: Symptoms, Transmission, and Treatment
Hepatitis B is a significant global health issue, caused by the Hepatitis B virus (HBV), which infects the liver and can lead to serious conditions such as liver cirrhosis and liver cancer if not managed properly. This article provides an overview of the symptoms, modes of transmission, available treatments, and preventive measures for Hepatitis B, as outlined by the Centers for Disease Control and Prevention (CDC).
What is Hepatitis B Virus (HBV)?
Hepatitis B virus (HBV) is a DNA virus classified within the Hepadnaviridae family, known for its compact and highly efficient genome that includes four overlapping open reading frames and a unique replication strategy involving reverse transcription. It’s enveloped, which enhances its ability to evade the host immune system, and it specifically infects liver cells (hepatocytes), leading to a range of hepatic disorders. The virus can exist in both acute and chronic forms, the latter posing a risk for serious conditions such as cirrhosis and hepatocellular carcinoma.
Covalently closed circular DNA (cccDNA) is a critical molecular form of the Hepatitis B virus (HBV) that serves as a viral persistence reservoir within the nucleus of infected hepatocytes. It functions as a template for viral transcription, contributing to the chronicity of HBV infection. The stability and longevity of cccDNA in liver cells make it a major challenge for the eradication of HBV, as it can remain dormant and then reactivate, complicating treatment efforts and sustaining infection even after apparent recovery.
Hepatitis B Transmission
Hepatitis B is transmitted through contact with infectious body fluids, such as blood, semen, and other bodily fluids from an infected person. Common modes of transmission include mother-to-child transmission at birth, sharing needles, syringes, or other drug-injection equipment, unprotected sexual contact with an infected partner, and transfusions of unscreened blood. Understanding these pathways is crucial for preventing the spread of the virus.
Hepatitis B Risk Factors
Several factors increase the risk for hepatitis B (HBV) infection. These include being born to a mother who is hepatitis B surface antigen (HBsAg) positive, living in or having parents from regions with high HBV prevalence, engaging in injection drug use, being incarcerated, having HIV or hepatitis C, being a man who has sex with men, having multiple sexual partners or sexually transmitted infections, living in the same household as someone with HBV, sharing needles, undergoing maintenance dialysis, and having elevated liver enzymes without a known cause.
Hepatitis B Symptoms
Symptoms of acute Hepatitis B virus (HBV) infection vary by age; infants and young children, as well as immunosuppressed adults, often show no symptoms. Older individuals, particularly those aged 30 and above, are more likely to experience symptoms. These can include fever, fatigue, loss of appetite, nausea, vomiting, abdominal pain, dark urine, clay-colored stools, joint pain, and jaundice. Chronic HBV often remains asymptomatic, though some may develop liver complications.
What is the incubation period for hepatitis B?
If symptoms occur, they begin an average of 90 days (range: 60–150 days) after exposure to HBV.
When symptoms of acute hepatitis B occur, how long do they usually last?
Symptoms typically last for several weeks but can persist for up to 6 months.
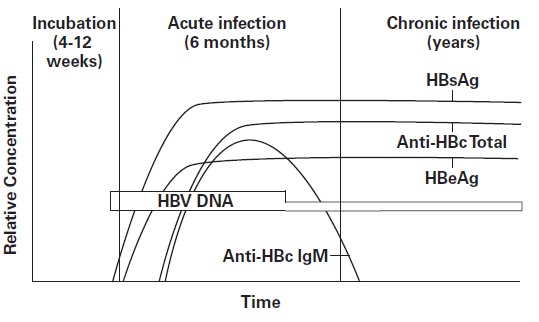
Hepatitis B Tests
For hepatitis B testing, the recommended seromarkers for adults include the triple panel: hepatitis B surface antigen (HBsAg), antibody to hepatitis B surface antigen (anti-HBs), and total antibody to hepatitis B core antigen (total anti-HBc). Infants born to HBsAg-positive individuals should be tested for HBsAg and anti-HBs. All pregnant individuals should be screened for HBsAg during each pregnancy, preferably in the first trimester, regardless of previous vaccinations or screenings. Those with a prior triple panel screening without new HBV exposure risks should only be tested for HBsAg.
Liver function tests (LFTs) are crucial in monitoring liver health in individuals with Hepatitis B virus (HBV) infection. These tests measure levels of liver enzymes such as alanine aminotransferase (ALT) and aspartate aminotransferase (AST), which are elevated when liver cells are damaged. Bilirubin and albumin levels are also checked to assess liver function. Regular monitoring through LFTs helps gauge the severity of infection, the degree of liver damage, and the response to HBV treatment strategies.
Hepatitis B Treatment
While there is no definitive cure for Hepatitis B, there are treatments available that can significantly reduce the risk of developing chronic disease and improve long-term outcomes. Antiviral medications like tenofovir and entecavir can help fight the virus and slow its ability to damage the liver. These treatments are particularly effective in chronic Hepatitis B cases and are recommended based on the phase of infection and the degree of liver damage.
CDC Hepatitis B Guidelines
The Centers for Disease Control and Prevention (CDC) has established updated guidelines for the screening and testing of Hepatitis B to enhance early detection and treatment, thereby reducing the public health burden of the disease. Here’s a summary of these recommendations:
- Universal Adult Screening: All adults should undergo Hepatitis B screening at least once in their lifetime using a triple panel test. This test includes the hepatitis B surface antigen (HBsAg), antibody to hepatitis B surface antigen (anti-HBs), and total antibody to hepatitis B core antigen (total anti-HBc). This approach aims to identify infected individuals early and link them to necessary care.
- Pregnant Individuals: It is recommended that all pregnant individuals be screened for Hepatitis B using the triple panel test, preferably during the first trimester of each pregnancy. This screening is vital regardless of previous vaccination or testing history, as it ensures timely prophylaxis for exposed infants and reduces vertical transmission rates.
- High-Risk Populations: Enhanced and periodic testing is advised for individuals with identified risk factors, regardless of age. These risk factors include a history of sexually transmitted infections, multiple sexual partners, incarceration, hepatitis C infection, injection drug use, and living with HIV, among others. Regular testing for these groups helps manage potential exposures and maintain health monitoring for those who remain unvaccinated.
- Vaccination Recommendations: Alongside testing, the CDC emphasizes the importance of hepatitis B vaccination as the most effective preventive measure against the virus. All unvaccinated adults up to age 59 years are advised to receive the Hepatitis B vaccine, with continued recommendations for older adults based on their risk exposure.
These measures are part of the CDC’s broader efforts to eliminate viral hepatitis as a public health threat and underscore the importance of broad access to screening and vaccination services. The guidelines aim to simplify the testing process, reduce the stigma associated with disclosure of risk factors, and ensure that more individuals with Hepatitis B can receive timely diagnosis and care.
For more detailed guidance and updates, visiting the CDC’s official page on Hepatitis B is recommended.
Booster Dose for Hepatitis B
For those who have been vaccinated, the immunity can decrease over time. In certain cases, a booster dose may be recommended to maintain immunity against the virus. Healthcare providers assess the necessity for a booster dose based on individual immune response and exposure risk to Hepatitis B virus.
Preventive Measures
The most effective way to prevent Hepatitis B is through vaccination, which is available and recommended for all infants at birth, followed by two or three more doses in the first six months of life. Adults who are at high risk of infection due to factors like occupation, travel to high-risk areas, or certain health conditions, should also get vaccinated.
For healthcare providers, adhering to standard precautions, including proper handling of needles and other sharp instruments, is crucial. Additionally, educating people about avoiding unprotected sexual contact and sharing needles can help reduce transmission.
In conclusion, while Hepatitis B remains a major public health challenge, effective preventive measures, thorough understanding of transmission routes, and available treatments provide significant means to manage and reduce the impacts of the disease. For more detailed guidance or management of Hepatitis B, contacting health professionals like Dr. Christos Zavos can provide personalized care and advice. Dr. Zavos can be reached through his website at peptiko.gr, by phone, or email, ensuring that individuals receive the best possible care tailored to their health needs.
