Autoimmune Hepatitis: A Chronic Liver Disease with Diverse Clinical Presentations
Autoimmune hepatitis (AIH) is a chronic, progressive disease characterized by immune-mediated inflammation of the liver. This condition can affect anyone regardless of age or background, but it predominantly affects females, with studies showing a female to male ratio ranging between 71% and 95% in adults diagnosed in the United States. AIH appears most commonly in two age groups—during the second and fifth decades of life—indicating a bimodal age distribution for this disease.
Subtypes and Autoantibodies
AIH is categorized into two main subtypes based on the patterns of specific autoantibodies present in the blood. Type 1 AIH, which constitutes approximately 96% of cases in US adults, and the less common Type 2 AIH, are distinguished by their different autoantibodies, which help in diagnosing and managing the disease.
Clinical Manifestations
The symptoms of AIH range significantly, from being completely asymptomatic to severe presentations that can lead to acute liver failure or cirrhosis. About 28-33% of adults with AIH already exhibit signs of cirrhosis at the time of their diagnosis. Symptoms, when present, are often nonspecific and can include fatigue, nausea, and abdominal pain. In severe cases, patients may exhibit jaundice and other signs of advanced liver disease such as spider nevi, palmar erythema, and splenomegaly. Additionally, AIH can coexist with other autoimmune disorders like vitiligo, inflammatory bowel disease, or autoimmune thyroid disease, complicating the clinical picture and diagnostic process.
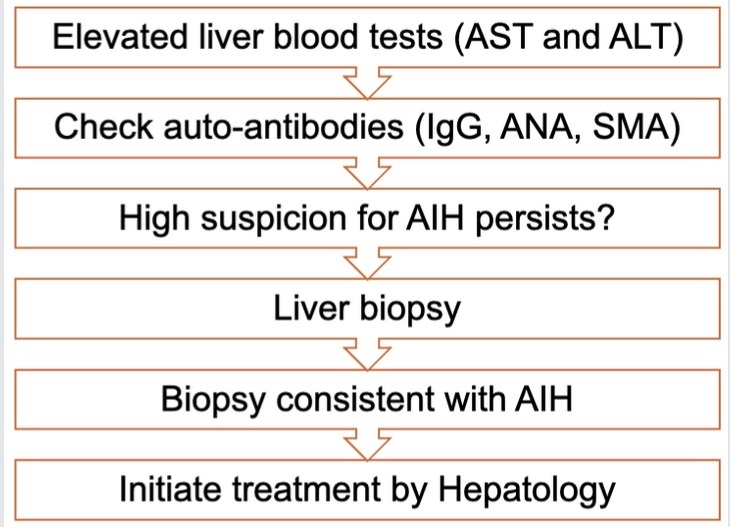
Diagnostic Process
The initial suspicion of AIH often arises following an elevation in liver enzymes detected during routine tests or tests performed due to unrelated symptoms. Further investigation typically reveals elevated serum levels of Immunoglobulin G (IgG). To diagnose AIH, physicians must first rule out other liver diseases such as viral hepatitis, drug-induced liver injury, and metabolic dysfunction-associated steatotic liver disease (MASLD). This is followed by testing for autoantibodies like anti-nuclear antibody (ANA) and anti-smooth muscle antibody (ASMA) in adults, and additional markers in children, such as anti-liver-kidney microsomal type 1 (LKM1) antibody.
Liver Biopsy and Histology
A liver biopsy remains key in confirming the diagnosis of AIH, particularly when serologic tests do not conclusively indicate the disease. The biopsy typically shows interface hepatitis with plasma cell infiltration, a hallmark of AIH. However, about 20% of AIH patients do not exhibit these autoantibodies, referred to as seronegative AIH, which further underscores the importance of a biopsy in the diagnostic process.
Treatment and Management
Autoimmune hepatitis (AIH) is a complex disease requiring careful management to regulate the immune system’s dysfunction. The primary approach involves immunosuppressive therapy to mitigate the overactive immune response targeting the liver.
First-Line Treatments
Oral glucocorticoids, such as prednisone and prednisolone, along with thiopurines like azathioprine, represent the cornerstone of AIH treatment. These drugs are effective in reducing liver inflammation and are the first choice in managing the condition.
Additional Therapeutic Options
In cases where patients exhibit intolerance to the first-line medications or if these treatments fail to achieve the desired response, alternatives such as mycophenolate mofetil, calcineurin inhibitors, and biologics may be considered. These options provide additional pathways to manage the disease, especially in more severe or treatment-resistant cases.
Monitoring Response to Therapy
The effectiveness of the treatment is monitored through regular assessments of liver enzyme levels (ALT and AST) and Immunoglobulin G (IgG). The goal of treatment is to improve these values, ideally normalizing them, indicating a controlled state of the disease. Patients with a high suspicion of AIH should be referred to a specialist in Hepatology to discuss the necessity of a liver biopsy and to outline potential treatment strategies.
Pre-Treatment Considerations
Before initiating treatment, several preparatory steps are recommended to minimize potential side effects and optimize patient outcomes:
- Thiopurine Methyltransferase (TPMT) Testing: This test is crucial to identify individuals at risk of severe myelosuppression from azathioprine, allowing for tailored therapy that avoids severe adverse reactions.
- Vaccinations: It is advisable to ensure that patients are up-to-date with age-specific vaccinations, including immunization against hepatitis A and B if they are not already immune. This preventive measure is critical to avoid further complications.
- Bone Health: Patients are at risk of osteoporosis from prolonged use of glucocorticoids. Therefore, bone density assessments are recommended, along with checks for Vitamin D levels at diagnosis and on an annual basis thereafter.
- Screening for Co-existing Conditions: Given the overlap with other autoimmune disorders, screening for conditions such as celiac disease and thyroid disorders is also recommended.
- Metabolic Syndrome Management: Monitoring and managing features of metabolic syndrome are crucial, as these can impact the overall health and treatment outcomes for patients with AIH.
- Psychological Support: Assessing psychological barriers to long-term medication adherence is vital, as depression and anxiety are more prevalent in AIH patients than in the general population. Addressing these issues can significantly impact treatment adherence and effectiveness.
Conclusion
Autoimmune hepatitis is a complex liver disease with a diverse range of presentations and significant implications for affected individuals. Due to its subtle onset and the severe consequences of delayed diagnosis, AIH requires a high degree of clinical awareness and timely intervention. Ongoing research and improved diagnostic strategies continue to enhance our understanding and management of this challenging autoimmune disorder, aiming to improve life quality and outcomes for those affected.
Understanding diseases like AIH underscores the need for comprehensive medical knowledge and awareness among gastroenterologists to ensure accurate diagnosis and effective management of such complex conditions.
